Daily cup of coffee may prevent afib recurrence
Gene-editing therapy lowers harmful blood fats in early study

What is EMDR therapy, and who can it help?

GLP-1 drugs versus bariatric surgery for treating obesity

Trying to lose weight? Be careful not to lose muscle

Two dumbbells, three exercises, and 10 minutes

Easing the emotional burden of IBS

Modify your push-ups to meet your fitness level

What is long QT syndrome?

Stroke survivors may benefit from very low LDL levels
Breast Cancer Archive
Articles
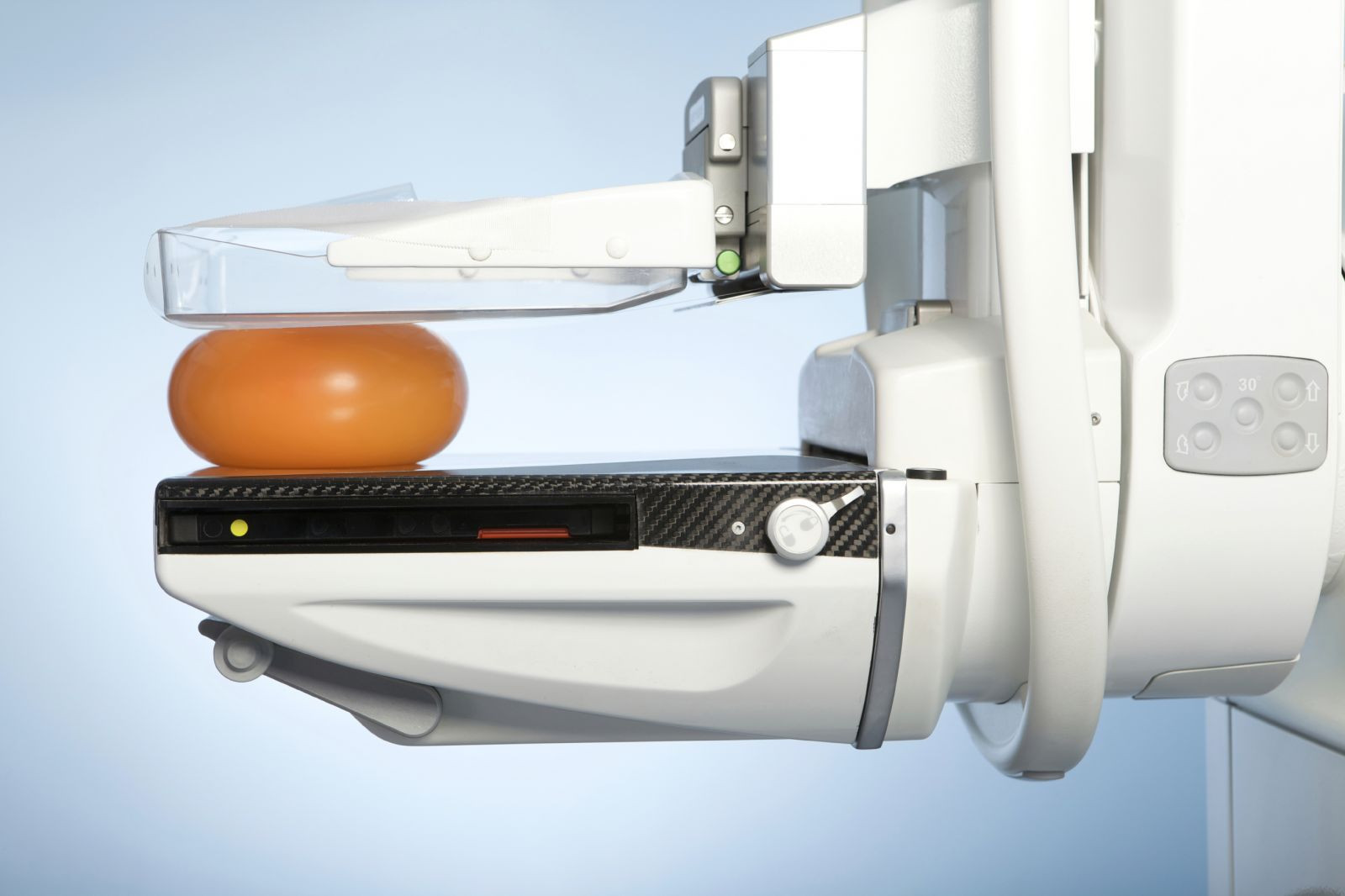
Should you still have mammograms after age 75?
The decision depends on several factors, including your breast cancer risk, life expectancy, and personal preferences.
Image: © Auremar/Thinkstock
As you get older, your body isn't the only thing that's changing. So are the guidelines for taking care of it. Breast cancer screening guidelines are a case in point. The current U.S. Preventive Services Task Force (USPSTF) guidelines recommend a mammogram every two years for women ages 50 to 75 with an average risk of developing breast cancer. For older women, the USPSTF said there isn't enough evidence of the potential risks and benefits of mammography on which to base a recommendation.
Although breast cancer is a leading cause of death in older women, women over 75 haven't been included in studies of mammography. However, there is evidence that most breast cancers detected in older women are relatively slow growing and easily treated. While a mammogram performed today might detect a cancer that would not spread or metastasize for several years, the percentage of women who survive to that point decreases with each passing year.
Postmenopausal women treated for DCIS live as long as other women
Research we're watching
Ductal carcinoma in situ (DCIS) differs from breast cancer because it is noninvasive, so it cannot spread to other parts of the body. However, it can progress to an invasive breast cancer, which can be life-threatening. Researchers from the Netherlands Cancer Institute wanted to determine how DCIS affected long-term survival.
The team studied almost 10,000 postmenopausal women who were diagnosed with DCIS between 1989 and 2004. They tracked the patients over an average of 10 years and compared their death rates with the expected mortality rates of the general population. They found that women who had been treated for DCIS had a 2.5% risk of dying of breast cancer over 10 years and a 4% risk at 15 years — rates that were higher than in the general population. But they also found that DCIS survivors had a 10% lower risk of dying from any cause compared with the general population. They presented their results Jan. 27, 2017, at the European Cancer Congress.
Why isn't there a more comfortable mammogram procedure?
Ask the doctor
Q. I have been smashed, squashed, pulled, and tugged annually for 25 years. Why isn't there a better way to take a mammogram?
A. We hear you! Compression mammography has been the "gold standard" for decades for one reason — it works. Flattening the breast makes ductal tissue easier to distinguish and reduces the amount of radiation required to do so. Studies have demonstrated that it is the most effective approach to breast cancer screening.
Many preventive mastectomies may be unnecessary
Women with early cancer in one breast may opt to remove the other, healthy breast because they overestimate their risk of a second cancer.
Electroacupuncture may ease hot flashes, aid sleep in breast cancer survivors
Electroacupuncture may be an effective alternative to medication for relieving hot flashes causing sleep disturbances in postmenopausal women.
Six things you should know about breast cancer risk
There's no one big way to reduce your risk for breast cancer, but a combination of approaches could make a difference.
In recent years the statistical picture of breast cancer has brightened, thanks to early detection and advances in treatment. More tumors are being caught at an early stage; the rise in incidence of the disease has slowed; and the death rate has dropped. Nevertheless, breast cancer is still the most commonly diagnosed cancer in women and the second most likely (after lung cancer) to take their lives.
Data aside, breast cancer looms large in our health concerns because most of us know it personally. Some of us have had the disease ourselves, and others have experienced it through friends or relatives. Particularly unsettling is its seeming randomness: Nothing seems to explain why one woman develops breast cancer and another doesn't. Granted, family history and certain gene mutations can substantially increase risk. But such factors aren't involved in most breast cancers. Moreover, we can't do much about them, or about many of the other risks associated with the disease, including older age (the 10-year risk of developing breast cancer jumps from 1 in 48 at age 40 to 1 in 26 at age 60), early menarche (first menstrual period), having no children (or bearing the first at a later age), and late menopause.
Adapting to life after cancer
Once you've completed treatment, adjusting to a "new normal" can be challenging.
Image: RuslaGuzov/ Thinkstock
Completing cancer therapy can feel like a graduation. You've done some hard work, it's paid off, and you may be ready to celebrate. But saying goodbye to treatment can arouse many of the emotions and uncertainties associated with beginning a new chapter in life.
Dr. Larissa Nekhlyudov is a general internist who works with cancer survivors at two Harvard affiliates, Brigham and Women's Hospital and Dana-Farber Cancer Institute. She acknowledges that cancer survivors have a lot to deal with. "Once you've had your final chemotherapy infusion or swallowed the last pill, you may find yourself facing a new set of challenges—monitoring yourself for signs of recurrence, getting recommended follow-up care, adjusting to the long-term effects of treatment, psychologically adapting to normal life, and working to stay in good health," Dr. Nekhlyudov says.
Dense-breast notification letters are confusing, study shows
Letters notifying women that they have dense breasts are difficult to understand. Women receiving them should contact their doctors.
Thyroid disease and breast cancer: Is there a link?
Researchers have wondered for a long time whether there might be a link between excess thyroid hormone and an increased risk of breast cancer. High levels of thyroid hormone have been shown to mimic estrogen, which fuels many breast cancers. A new study has suggested that there may indeed be a link — but it’s important to put the results into context.
Breast cancer: The good news
Personalizing breast cancer diagnosis and treatment has resulted in therapies that are more effective and less toxic than in the past.
Image: Thinkstock
The federal government's "Cancer Moonshot," with the expressed goal of curing cancer, is getting a lot of press lately. While the initiative's stated goal may be overly ambitious because cancer is actually 200 or more individual diseases, it promises to increase research funding and speed the availability of new treatments.
Amid the excitement, it's easy to overlook the fact that there has already been great progress in treating many cancers. Patients are enduring fewer side effects and living longer. Breast cancer is a prime example. "There's no question that breast cancer treatment is improving," says Dr. Ann Partridge, senior physician at the Susan F. Smith Center for Women's Cancers at Harvard-affiliated Dana-Farber Cancer Institute.

Daily cup of coffee may prevent afib recurrence
Gene-editing therapy lowers harmful blood fats in early study

What is EMDR therapy, and who can it help?

GLP-1 drugs versus bariatric surgery for treating obesity

Trying to lose weight? Be careful not to lose muscle

Two dumbbells, three exercises, and 10 minutes

Easing the emotional burden of IBS

Modify your push-ups to meet your fitness level

What is long QT syndrome?

Stroke survivors may benefit from very low LDL levels
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up