Trying to lose weight? Be careful not to lose muscle

Is your skin problem actually an autoimmune condition?

People with diabetes face higher risk of hearing loss

Antibiotic-free fixes for recurrent UTIs

Musculoskeletal syndrome of menopause: When menopause makes you ache all over

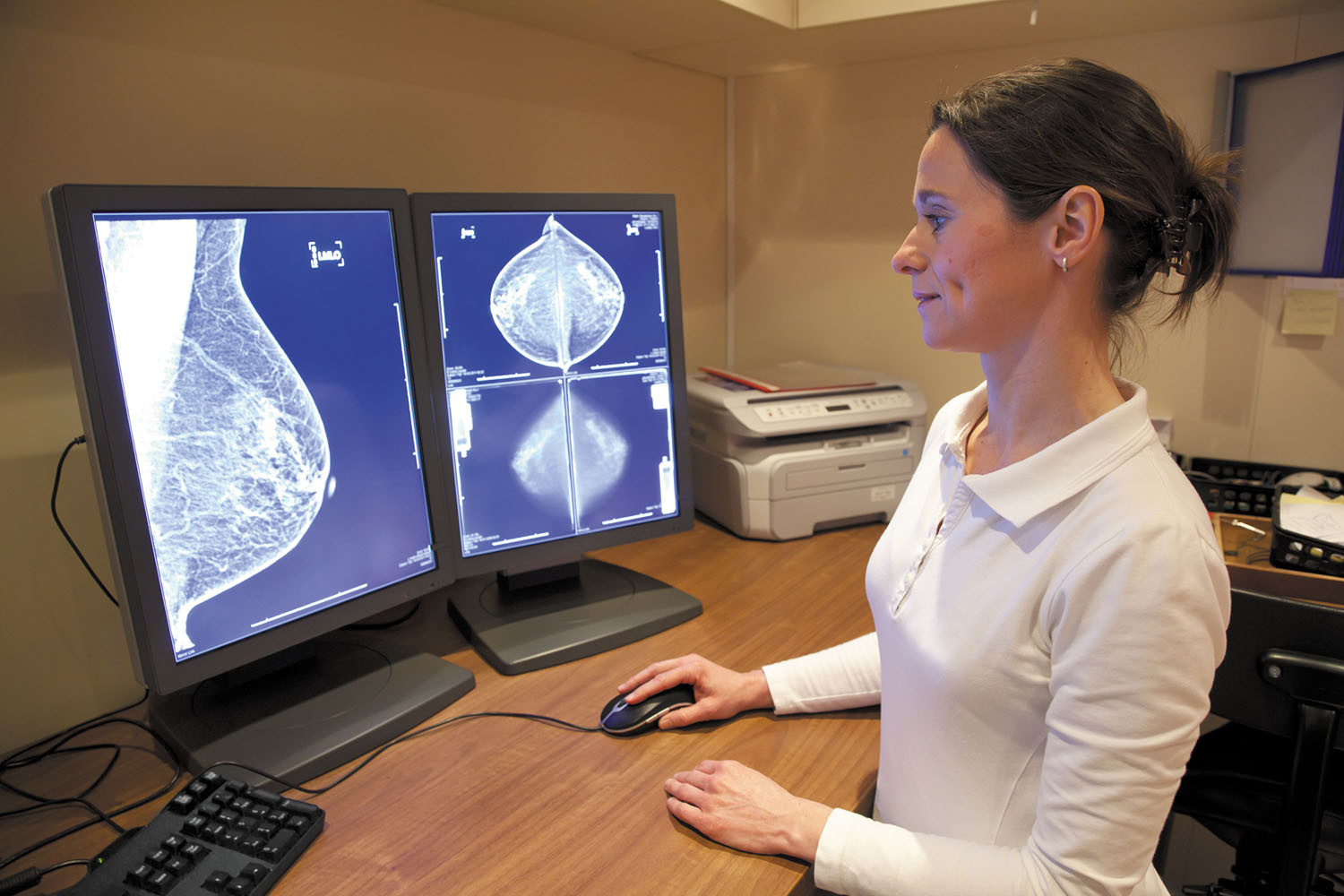
When can older women stop getting mammograms?

To lose weight, especially harmful belly fat, combine diet and exercise

Can men hold off on treating recurring prostate cancer?

The 7 types of rest and why we need them all

What are the early warning signs of cervical cancer?
Women's Health Archive
Articles
10,000 steps a day — or fewer?
If you’re trying to take 10,000 steps a day, it can be discouraging to miss that well-known target. But why is 10,000 steps the goal? And is it really necessary to take that many steps every day?
4 behavioral changes to tame urinary incontinence
The discomfort and potential embarrassment of urinary incontinence keeps many people from the activities they enjoy, but some simple behavioral changes can improve bladder control.
What is a submucosal uterine fibroid?
Ask the doctors
Q. I was recently diagnosed with a uterine fibroid. My doctor told me that the type I have is called a submucosal fibroid. What does this mean?
A. Uterine fibroids are common, affecting some 70% or more women. Doctors describe fibroids based on where in the uterus they are growing. There are three main types:
How can I prevent recurrent UTIs?
Ask the doctors
Q. I am 89 years old, and several months ago I was plagued by frequent urinary tract infections. The infections were treated, but is there anything I can do to avoid experiencing this problem again?
A. Urinary tract infections, or UTIs, are common infections that can occur when urine pools in the bladder and bacteria start to grow. These infections can be more common in older women for several reasons, including thinning of vaginal tissue, pelvic organ prolapse, incontinence, or difficulty with emptying the bladder completely. In addition, estrogen helps to maintain a healthy balance of bacteria in the vagina, which can protect against UTIs. But this natural protection may wane when estrogen levels drop after menopause. One of the best ways to prevent UTIs is to stay hydrated by drinking plenty of water. This flushes out potentially harmful bacteria before it can cause a problem. You'll know you are drinking enough if your urine looks clear or light yellow. Some other strategies include fully emptying your bladder when urinating, urinating after sexual intercourse, and wiping from front to back after using the toilet. Also talk to your doctor about replacing estrogen in the vagina with a cream, tablet, or vaginal insert. Your doctor may also want to examine you for pelvic organ prolapse.
Dealing with high-density breasts
The FDA may require mammography facilities to notify patients about this breast cancer risk factor, but women don't know what to do with this information.
Do you know how dense your breasts are? If you don't, a new proposal by the FDA may mean you will soon find out.
The agency proposed a change that, if approved, will require mammography facilities to send letters informing women about their breast density — a measure of the proportion of active tissue versus fat in their breasts (see "The FDA proposal").
FDA takes some surgical mesh products off the market
Research we're watching
Transvaginal mesh, which has been used in transvaginal pelvic organ prolapse procedures since the 1990s, can no longer be sold in the United States because of concerns over safety and efficacy, according to the FDA. The number of women reporting problems related to these mesh products has grown over the past several years. The FDA said it made the decision because the companies that manufacture the mesh couldn't demonstrate that surgical procedures with their products work better than those without the mesh. They also failed to submit evidence that the mesh is safe and effective over the long term, said the FDA.
Women who have had procedures using mesh and are experiencing complications such as groin pain, persistent vaginal bleeding, pain during sex, or vaginal discharge should notify their doctor. Women who had procedures using mesh but aren't having any issues don't need to take any action aside from having their usual check-ups, said the FDA.
By the way, doctor: My Pap tests show insufficient cells. What does that mean?
Q. For two years in a row, the lab that handles my Pap smears has reported "insufficient cell count." My doctor says it's nothing to worry about, but my health insurance company considers these "abnormal" Paps and has put me in a higher-risk category because of it. Should I be concerned?
A. When lab pathologists evaluate Pap tests for abnormal cells, the goals are to identify cancer that should be removed and precancerous conditions that should be followed closely to watch for any changes. Sometimes the results are unclear because the lab sample doesn't contain enough cells to evaluate ("insufficient cell count") — or because the cells are obscured by inflammation, mucus, or blood from a heavy menstrual period. In these cases, the Pap test is not necessarily abnormal; the specimen is simply inadequate to make any determination.
Managing postmenopausal vaginal atrophy
Vaginal dryness is one of the most irritating symptoms of menopause. Here are some ways to relieve it.
Within a few years of menopause, roughly 50% of women develop symptoms related to vaginal atrophy, also called atrophic vaginitis — the deterioration of vaginal tissues due to loss of estrogen. The most common symptoms of vaginal atrophy are dryness, irritation, and pain during intercourse.
Although menopause is the most common cause, vaginal atrophy can result from anything that lowers estrogen production. That includes chemotherapy, radiation, removal of the ovaries during hysterectomy, and use of anti-estrogenic therapies such as aromatase inhibitors, tamoxifen (Nolvadex), and drugs like leuprolide (Lupron) and nafarelin (Synarel), which are used to treat fibroids and endometriosis. Unlike hot flashes, which usually subside with time, vaginal atrophy is likely to persist and become worse without treatment.

Trying to lose weight? Be careful not to lose muscle

Is your skin problem actually an autoimmune condition?

People with diabetes face higher risk of hearing loss

Antibiotic-free fixes for recurrent UTIs

Musculoskeletal syndrome of menopause: When menopause makes you ache all over

When can older women stop getting mammograms?

To lose weight, especially harmful belly fat, combine diet and exercise

Can men hold off on treating recurring prostate cancer?

The 7 types of rest and why we need them all

What are the early warning signs of cervical cancer?
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up