Driving with arthritis pain: Stay comfortable — and safe — behind the wheel

Daily cup of coffee may prevent afib recurrence

Gene-editing therapy lowers harmful blood fats in early study

What is EMDR therapy, and who can it help?

GLP-1 drugs versus bariatric surgery for treating obesity

Two dumbbells, three exercises, and 10 minutes

Easing the emotional burden of IBS

Modify your push-ups to meet your fitness level

What is long QT syndrome?

Stroke survivors may benefit from very low LDL levels
Bladder & Bowel Archive
Articles
Can I do anything to prevent urinary incontinence?
Ask the doctors
Q. I'm hoping to prevent urinary incontinence. Is there anything I can do?
A. Nearly half of all women experience some type of urinary incontinence during the course of their lives. It may not be possible to prevent all of these cases, which can be caused by pregnancy, childbirth, or hormonal shifts that occur around the time of menopause. Here are some strategies that may help to reduce your risk.
When should I be concerned about the color of my urine?
On call
Q. When should I worry about changes in the color of my urine? What color is considered healthy?
A. If a person is well hydrated, the normal color of urine is a pale yellow. Someone who drinks large amounts of fluid or takes diuretics (water pills) can have almost clear-looking urine. A dark yellow color may indicate a need to increase your fluid intake.
Behavioral therapy can relieve overactive bladder symptoms
In the journals
Men often rely on drugs to manage overactive bladder symptoms, such as frequent urination, urgency, incontinence, and nocturia (having to use the bathroom at night). However, a study published online Jan. 13, 2020, by JAMA Internal Medicine suggests that adding behavioral therapy may lead to better results.
Scientists recruited more than 200 men (average age 64) with overactive bladder symptoms and divided them randomly into three groups. One group received only drug therapy. One received only behavioral therapy, which consisted of learning pelvic floor exercises and relaxation techniques to help suppress urges and prevent urine loss. The third group had both behavioral and drug therapy.
5 ways to dodge incontinence
Most people take bladder control for granted — until the unintended loss of urine interrupts the ability to carry on an ordinary social and work life.
Often, the causes of incontinence are out of a person's control. For example, in women, incontinence is a common side effect of childbirth. For men, it's often a side effect of treatment for prostate problems.
Men and urinary tract infections
On call
Image: © KEMPSKI/Getty Images
Q. What causes urinary tract infections and are men at risk for getting them?
A. Although urinary tract infections (UTIs) are more common in women, men can get them, too. They occur when bacteria build up somewhere along your urinary tract. In men, UTIs can develop in the urethra (the tube that runs from the opening at the tip of the penis to the bladder), the bladder, the prostate, or the kidney.
Red, brown, green: Urine colors and what they might mean
Departures from the familiar yellow color of urine are often harmless but should be discussed with a doctor.
Most of the time, urine is a pale-yellow color because it contains urochrome, one of the substances produced when hemoglobin gets broken down. Hemoglobin is the protein in red blood cells that sticks to oxygen so it can be ferried around the body.
Occasionally, though, urine turns a very different color. Men may notice the change as their urine enters the toilet bowl or urinal. Women may be more likely to observe it after wiping. Seeing red or orange instead of the usual yellow can be alarming, especially if there are also symptoms like a burning sensation or pain with urination. The alarm may be justified: an abnormal urine color can be an early sign of a serious medical condition. To be on the safe side, it should be discussed with a doctor or another clinician.
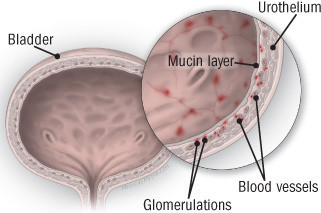
Diagnosing and treating interstitial cystitis
Also called painful bladder syndrome, this frustrating disorder disproportionately affects women.
Interstitial cystitis is a chronic bladder condition that causes recurring bouts of pain and pressure in the bladder and pelvic area, often accompanied by an urgent and frequent need to urinate — sometimes as often as 40, 50, or 60 times a day, around the clock. Discomfort associated with interstitial cystitis can be so excruciating that, according to surveys, only about half of people with the disorder work full-time. Because symptoms are so variable, experts today describe interstitial cystitis as a member of a group of disorders collectively referred to as interstitial cystitis/painful bladder syndrome. (In this article, we'll call it interstitial cystitis, or IC.)
Among the one to two million Americans with IC, women outnumber men by as much as eight to one, and most are diagnosed in their early 40s. Several other disorders are associated with IC, including allergies, migraine, irritable bowel syndrome, fibromyalgia (a condition causing muscle pain), chronic fatigue syndrome, and vulvodynia (pain or burning in the vulvar area that isn't caused by infection or skin disease).
What’s causing bladder pain or burning?
Infections aren't the only conditions that can cause discomfort.
Certain urinary symptoms are quite common, particularly in women: painful burning with urination, an urgent need to urinate like you can't hold it (urinary urgency), and urinating frequently (urinary frequency).
These symptoms can be caused by any of the following conditions.
Is bladder training really beneficial?
Ask the doctors
Q. I suffer from mild urinary incontinence. A friend suggested that I try bladder training. Is this a real treatment?
A. Yes, some women with urinary frequency and overactive bladder might benefit from bladder training. The idea behind bladder training is to teach your body to respond more appropriately to bladder signals.
What to do when medication makes you constipated
Antidepressants and opioids are common offenders.
It's frustrating when you feel the urge to move your bowels but can't seem to go. Before blaming your diet, consider whether medication side effects are causing your constipation.
Possible suspects
Many medications can contribute to constipation, including the following:

Driving with arthritis pain: Stay comfortable — and safe — behind the wheel

Daily cup of coffee may prevent afib recurrence

Gene-editing therapy lowers harmful blood fats in early study

What is EMDR therapy, and who can it help?

GLP-1 drugs versus bariatric surgery for treating obesity

Two dumbbells, three exercises, and 10 minutes

Easing the emotional burden of IBS

Modify your push-ups to meet your fitness level

What is long QT syndrome?

Stroke survivors may benefit from very low LDL levels
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up