Depression during pregnancy and after
For too many women, joyfully anticipated pregnancy and motherhood bring depression as an unexpected accompaniment. Children as well as mothers suffer. Depression during pregnancy may result in poor prenatal care, premature delivery, low birth weight, and, just possibly, depression in the child. Depression after childbirth (postpartum depression) can lead to child neglect, family breakdown, and suicide. A depressed mother may fail to bond emotionally with her newborn, raising the child's risk of later cognitive delays and emotional and behavior problems. Fortunately, if the depression is detected soon enough, help is available for mother and child.
Depression During Pregnancy
Depression in pregnant women is often overlooked, partly because of a widespread misconception that pregnancy somehow provides protection against mood disorders. In reality, almost 25% of cases of postpartum depression in womem start during pregnancy, and depression may peak at that time, according to a study published in the British Medical Journal.
More than 9,000 women recorded their moods during the fourth and eighth month of pregnancy and again two and eight months after giving birth. The questionnaire, which was specially designed for pregnant women and new mothers, concentrated on thoughts and feelings—emotional swings, crying spells, low self-esteem, hopelessness, irritability, and inability to enjoy normally pleasurable activities. The researchers paid less attention to physical symptoms, because they did not want to mistake physical effects of pregnancy (such as appetite loss, fatigue, and insomnia) for symptoms of depression. Depression ratings were highest at the eighth month of pregnancy and lowest eight months after childbirth. Fourteen percent of the women scored above the threshold for probable clinical depression just before the child's birth, compared with 9% two months later.
Ignoring depression during pregnancy can be risky for both mother and child. Depressed women often take poor care of themselves. They may smoke, drink to excess, or neglect proper diet. And some research suggests that depression in pregnant women can have direct effects on the fetus. Their babies are often irritable and lethargic, with irregular sleep habits. These newborns may grow into infants who are underweight, slow learners, and emotionally unresponsive, with behavior problems such as aggression.
Depression After Childbirth
Postpartum depression in women is usually divided into three categories: baby blues, nonpsychotic postpartum depression, and postpartum psychosis.
Baby blues, the most common mood disturbance after childbirth, may affect nearly 50% of new mothers. The cause of this usually brief and harmless condition may be hormonal changes, especially the rapid fall in estrogen levels after birth. Some symptoms are appetite loss, fatigue, confusion, sadness, nervousness, crying spells, oversensitivity, and a feeling of being overwhelmed. These symptoms appear within a few days of delivery and subside in about two weeks. If they last longer, a woman may be suffering from clinical depression, a condition that occurs in 10%–15% of new mothers.
The American Psychiatric Association defines "depression with postpartum onset" as a depressive episode that occurs within four weeks of birth, but many researchers regard the postpartum period as lasting up to six months after delivery. Women have a higher than average rate of hospital admissions for depression during this period and for as long as three years after childbirth. The symptoms may include headaches, chest pain, heart palpitations, and panic attacks as well as fatigue, sadness, hopelessness, irritability, and loss of interest and pleasure in life. Often worrying obsessively about the child's health, depressed women feel guilty about their inadequacy as caregivers—and even about not being as happy as they think they should be.
Mood disorders, either major depression or bipolar disorder, are the most common cause of maternal psychosis, with delusions, hallucinations, or both. The danger is especially great when delusions center on the baby. Many mothers with postpartum depression are afraid they will harm the baby. Few actually do, but the risk is greater if the woman is psychotic. A woman who suffers a psychotic postpartum depression once is likely to have similar episodes after the birth of other children.
The Child's Response
A mother's depression itself can make some of her worries about her child realistic. Infants are highly sensitive to a mother's sadness, silence, and inattentiveness. In one study, mothers of 3-month-old infants were asked to simulate depression for three minutes. They spoke in a monotone, remained expressionless, and avoided touching the child. Even at that age infants could respond to fleeting changes in their mothers' apparent mood. They looked away from their mothers and showed signs of distress, which continued for a time even after the women began to behave normally.
In the long run, child development may be affected. Children of depressed parents in general are highly vulnerable to depression, and long-term adjustment is sometimes a problem for the children of mothers with postpartum depression. In one study, teachers' reports were used to compare the children of 55 women with postpartum depression to the children of 40 healthy controls over a five-year period beginning a few months after childbirth. Boys from lower-class families were affected most. In that group, investigators found a higher than average rate of clinically significant behavior problems (chiefly hyperactivity and distractibility) after five years if and only if their mothers suffered from postpartum depression. With or without depressed mothers, serious behavior problems were rare in middle-class children.
Drug Therapy
Depressed women may be reluctant to seek help because they fear they will be regarded as bad mothers. Family doctors can help by reassuring them about their child's health and asking about depressive symptoms.
Antidepressant drugs are a standard treatment for depression during pregnancy and after birth, but many women are understandably worried about drug effects on the child. Some potential risks are birth defects, neonatal toxicity (jitteriness, difficulty in feeding, and irregular heart rate or breathing associated with exposure to a medication before or during delivery), and longer-term cognitive, emotional, or behavioral effects.
Some women who are already taking antidepressants may want to quit before conceiving a child, and some who become depressed while pregnant or nursing may prefer to avoid drugs. Much depends on how severe the depression is and how well both mother and child can cope with its symptoms. Pregnant and nursing women should be aware that prolonged depression may be riskier than drug side effects, both for themselves and for their children.
Other Treatments
Electroconvulsive therapy is a highly effective treatment for severe postpartum depression—especially psychotic depression. It can be safely administered a week after childbirth. The most important side effect is some loss of memory for the period immediately surrounding the treatment.
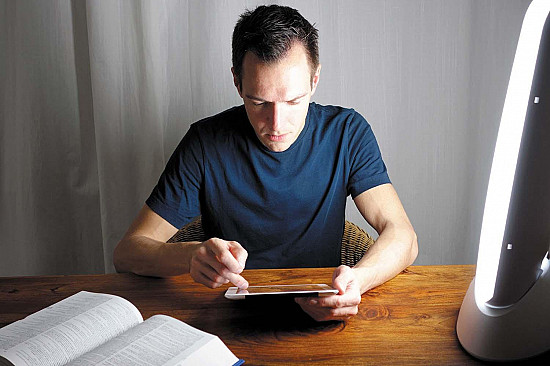
Another somatic (physical) treatment is bright light therapy (phototherapy). It is already thought to be effective for postpartum depression, and a trial reported in the American Journal of Psychiatry suggests that it is also an option for depression during pregnancy. Sixteen pregnant women with major depression sat close to a bright light source one hour a day for three to five weeks. Average depression ratings improved by 49% after three weeks and by 59% in the seven patients who had five weeks of treatment. When the treatment ended, their symptoms became worse. The results are promising, but controlled studies are needed.
Psychotherapy is a proven treatment for mild to moderate depression in three common forms: cognitive behavioral, psychodynamic, and interpersonal.
Interpersonal therapy may be especially useful for depression during pregnancy and the postpartum period because it is designed to help people cope with changing circumstances and social roles. Being constantly alone with an infant is not good for new mothers. Group therapy and self-help groups can provide needed companionship and advice, especially for a woman who has limited family contact or few other social outlets. Couples therapy may help when marital problems have been contributing to depression.
Researchers looking for ways to prevent depression are investigating risk factors during pregnancy and the postpartum period. An unplanned pregnancy, an unhappy marriage, or a child with a difficult temperament may raise the risk. Questionnaire responses by more than 5,000 Danish women indicate that emotional distress and social isolation during pregnancy are associated with postpartum depression. In another study, 38 new mothers answered questionnaires on fatigue and depression one day after giving birth and again after one, two, and four weeks. Women with a high level of fatigue after one and two weeks were more likely to report symptoms of depression after four weeks.
The studies reflect an understanding that depression among pregnant women and new mothers is a serious public health problem. The more effectively it is prevented and the sooner it is treated, the better the family environment and the more hopeful the outcome for both mother and child.
Resources:
Depression After Delivery, Inc.
91 East Somerset Street
Raritan, NJ 08869
Telephone: 800-944-4773 (toll free)
On the Web: http://www.depressionafterdelivery.com
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.