What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Medical Tests & Procedures Archive
Articles
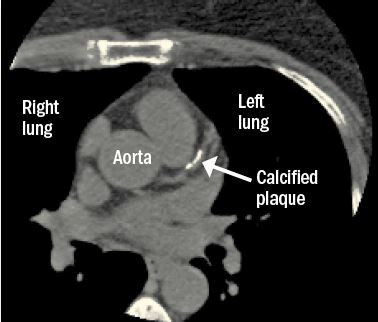
When you look for cancer, you might find heart disease
Screening tests for lung and breast cancer—chest computed tomography (CT) scans and mammograms—may offer clues about a person’s risk of heart disease.
Where to turn for low back pain relief
In most cases, a primary care doctor or chiropractor can help you resolve the problem.
Low back pain is one of the most common complaints on the planet. And you may wonder where to turn when you start experiencing some of those aches or twinges in the lower part of your back. Take heart. "In most cases, you won't need a specialist," says Dr. Robert Shmerling, a rheumatologist at Harvard-affiliated Beth Israel Deaconess Medical Center.
When pain strikes
There are many causes of low back pain. Some of the most common include an injury to a muscle or tendon (a strain), an injury to a back ligament (a sprain), and a herniated or "slipped" disc (when the soft material inside of a disc between spinal bones leaks and irritates nerves). Many of these issues will eventually resolve on their own.
What is a “full metal jacket”?
Ask the doctor
Image: © MileA/Thinkstock
Q. I heard my cardiologist say to another doctor that I have a "full metal jacket." What does that mean?
A. Cardiologists use the term "full metal jacket" to refer to a long series of stents in one of the heart's three major arteries. Stents are tiny metal cylinders, often with drug coatings, that help prop open arteries to restore blood flow to the heart. They're placed inside arteries during an angioplasty, in which a doctor snakes a thin, flexible tube (catheter) through the blood vessels to a narrowed section. A deflated balloon at the tip of the catheter then inflates, pushing fatty plaque against the artery wall and expanding the stent.
Should you stop anti-clotting drugs before a procedure?
Because many factors are involved, make sure your doctors talk to each other if you need an invasive test or procedure.
Image: © thodonal/Thinkstock
Millions of people with cardiovascular disease take drugs that help prevent blood clots, which can lodge in a vessel and choke off part of the blood supply to a leg, a lung, or the brain. These potentially lifesaving medications, known generally as anticoagulants, include warfarin (Coumadin) and a class of drugs called non–vitamin K antagonist oral anticoagulants, or NOACs (see "Anti-clotting drugs: The old and the new").
However, if you're taking one of these drugs and need an invasive procedure — anything from a tooth extraction to a hip replacement — managing the risks can be tricky, says cardiologist Dr. Gregory Piazza, assistant professor of medicine at Harvard Medical School. "There's a higher-than-normal risk of bleeding during and after the procedure, because your blood doesn't clot as easily," he says.
Laser procedure a possible treatment for eye floaters
In the journals
A common laser treatment may help people with a specific type of eye floater, according to a small study published online July 20, 2017, by JAMA Ophthalmology. Floaters are spots in your vision like black or gray specks, strings, flying bugs, or cobwebs. They become more prevalent with age and occur when the jelly-like substance inside the eyes becomes more liquid, shrinks, and separates from the back wall of the eye.
There are three treatments for floaters: observation, where a floater is monitored for changes (for instance, if it moves away from your central vision or the brain adapts and ignores it); vitrectomy surgery to remove the floater; and YAG vitreolysis, which vaporizes the floater with a laser.
Should you try a home genetic test kit?
A direct-to-consumer test can uncover risks for developing some diseases. But will it help you improve your health?
Image: © pe-art/Thinkstock
What if you could take a test at home to predict your risk of getting certain diseases, like Alzheimer's or Parkinson's? It's a question you may face now that the FDA has given the green light to third-party direct-to-consumer (DTC) test kits that look for genetic risk information.
"Increasingly, people want to explore their own medical data," says Dr. Robert Green, a Harvard Medical School professor and geneticist at Harvard-affiliated Brigham and Women's Hospital, who studies the medical, behavioral, and economic outcomes associated with genomic medicine (for more about his work, visit www.genomes2people.org).
When the heart pumps normally but struggles
Ask the doctor
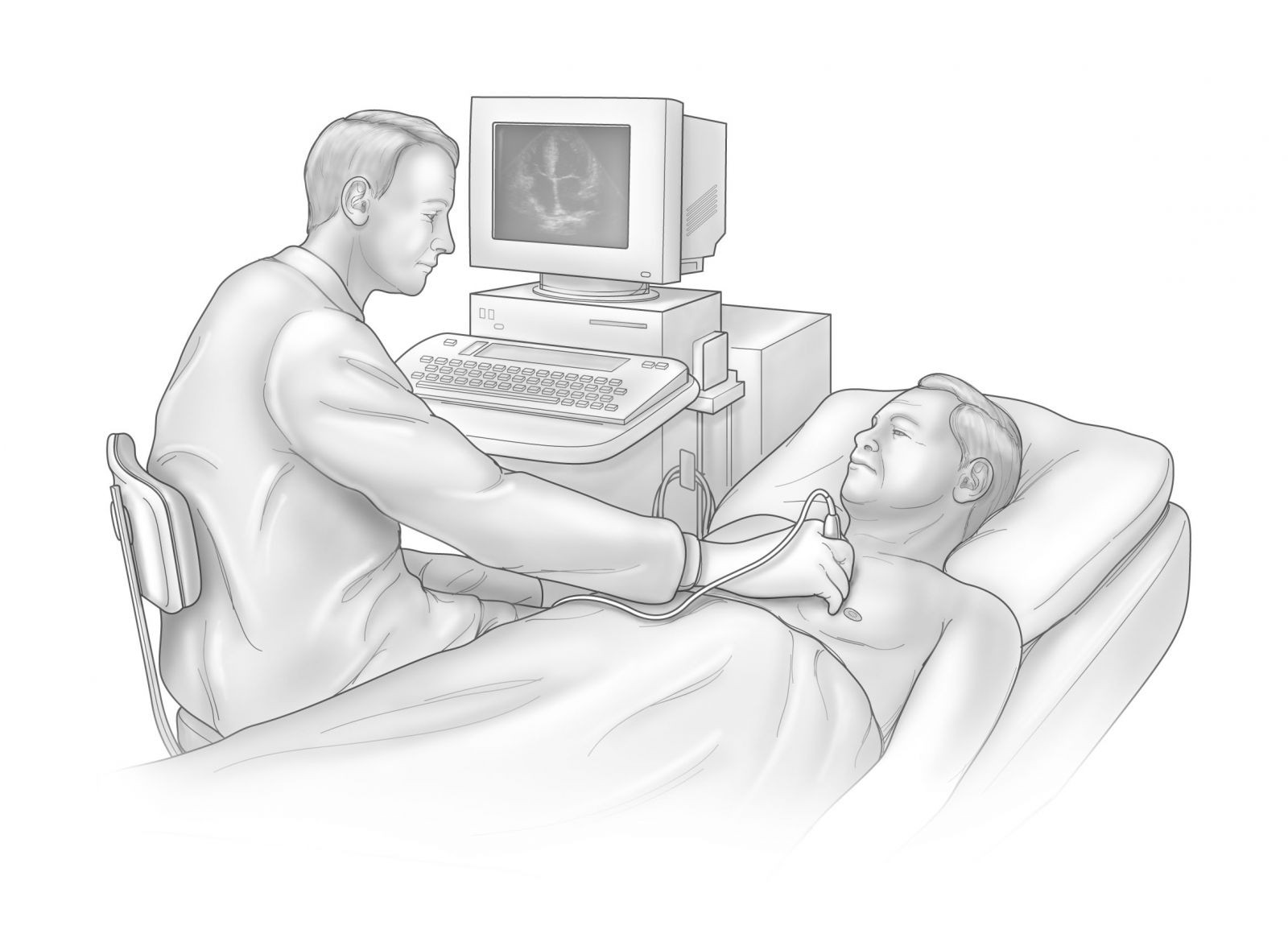
Illustration by Scott Leighton
Q. I was recently admitted to the hospital with heart failure and received a heart ultrasound. The test report stated that my heart's pumping ability is normal. I don't understand. Was my diagnosis wrong, or is the test wrong?
A. If you were diagnosed with heart failure in the hospital, I'm presuming that you were admitted with symptoms such as shortness of breath, fatigue, and difficulty doing everyday activities. Other common symptoms include swelling in your legs and feet and trouble breathing at night.
Does prostate cancer screening matter?
The latest guidelines suggest you should have an engaged conversation with your doctor about PSA testing.
Image: © Mark Bowden/Thinkstock
An annual prostate-specific antigen (PSA) test to check for signs of possible prostate cancer sounds innocent enough, but new guidelines suggest the test offers few long-term benefits, and substantial possible harm.
The updated guidelines from the U.S. Preventive Services Task Force (USPSTF), published online April 11, 2017, by The Journal of the American Medical Association, reinforce the organization's 2012 conclusion that PSA screenings have only a small potential benefit for reducing the chance of dying of prostate cancer for men ages 55 to 69 — while exposing them to possible overtreatment and side effects from biopsies, radiation, and surgery.
Clot prevention with a mechanical heart valve
Ask the doctor
Image: © Hailshadow/Thinkstock
Q. I have a mechanical heart valve, so I'm taking warfarin. But the frequent blood tests and occasional dose changes are bothersome. When, if ever, will I be able to take one of the new blood thinners instead of warfarin? Off-label use of other drugs is not uncommon. Why isn't that an option in this case?
A. Your question is a good one, and it requires a two-part answer. When doctors prescribe drugs "off-label," that means they believe the drug will help you, even if it has not been FDA-approved specifically for your condition. Sometimes, subsequent research provides strong evidence to support a specific off-label use, which may lead to the drug's FDA approval for that condition. But sometimes, research shows the exact opposite: a medication that doctors assumed would be beneficial is, in fact, not helpful — and sometimes even harmful.
Is advanced lipoprotein testing useful?
Ask the doctor
Image: © designer491/Thinkstock
Q. I'm a trim, healthy 57-year-old who exercises religiously, six days a week. I take a low-dose statin and my cholesterol numbers are pretty good (total cholesterol is 146, LDL is 77, and HDL is 51). But a recent blood test showed that my lipoprotein subfractions are not ideal: my small LDL and large HDL values are considered "high risk," according to the report I received. What can I do to improve my lipoprotein subfractions, and how important are they in the overall scheme of things?
A. It sounds like you had advanced lipoprotein testing, which is a more detailed and also more expensive version of a standard cholesterol or lipid test. In general, I'm not a fan of this type of testing, because there is no solid evidence that the results are useful in any concrete way or provide information that can improve a person's health. To understand why, a little background on cholesterol and its role in heart disease may be of help.

What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up