What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Medical Tests & Procedures Archive
Articles
Do you need a calcium scan?
This noninvasive test can predict plaque in the heart's arteries. But it is useful only in certain situations.
Imagine a 57-year-old man (let's call him Bill) who's in pretty good health — a nonsmoker who eats right and exercises regularly. He takes two drugs to treat high blood pressure. Even though his LDL (bad) cholesterol isn't all that high, his primary care doctor suggests that Bill consider taking a statin to lower his risk of a heart attack.
Bill is a little hesitant to add another drug to his daily regimen, so his doctor tells him about a test that may help with the decision: a coronary artery calcium scan. This noninvasive test, which can reveal dangerous plaque in the heart's arteries, has been available for more than a decade. But calcium scans (as they're often called) are now recognized in official guidelines and are being used far more often than in the past, says Dr. Ron Blankstein, a cardiovascular imaging specialist and preventive cardiologist at Harvard-affiliated Brigham and Women's Hospital.
Aspirin before colon cancer screening doesn't boost test accuracy
Aspirin falls short in improving colon cancer test results.
Closing in on tinnitus treatments
New research aims to capture and eventually cure incessant ringing in the ears.
More than 50 million Americans struggle with tinnitus, a constant or recurring ringing in the ears that ranges from irritating to debilitating. Some treatments work for some people, but none seems to work for everyone.
Tinnitus is a tough condition for doctors to study. "There's no way to measure it directly. The only way we know you have tinnitus is if you tell us. Even if there were a cure, we wouldn't know how it worked because we have to rely on verbal descriptions of what your tinnitus sounds like and how loud it is," says Daniel Polley, director of the Lauer Tinnitus Research Center at Harvard-affiliated Massachusetts Eye and Ear.
New insights about inflammation
Recent research reignited interest in inflammation, a major player in heart disease.
A buildup of cholesterol-rich plaque inside arteries — known as atherosclerosis — is the root cause of most heart attacks and strokes. Researchers have long recognized that chronic inflammation sparks this artery-damaging process (see "Understanding inflammation"). Now, they're zeroing in on better ways to tackle that aspect of the problem.
Addressing inflammation is vital. Even when people take steps to lower their risks for heart disease, such as reducing their cholesterol and blood pressure, they may still face life-threatening cardiovascular events.
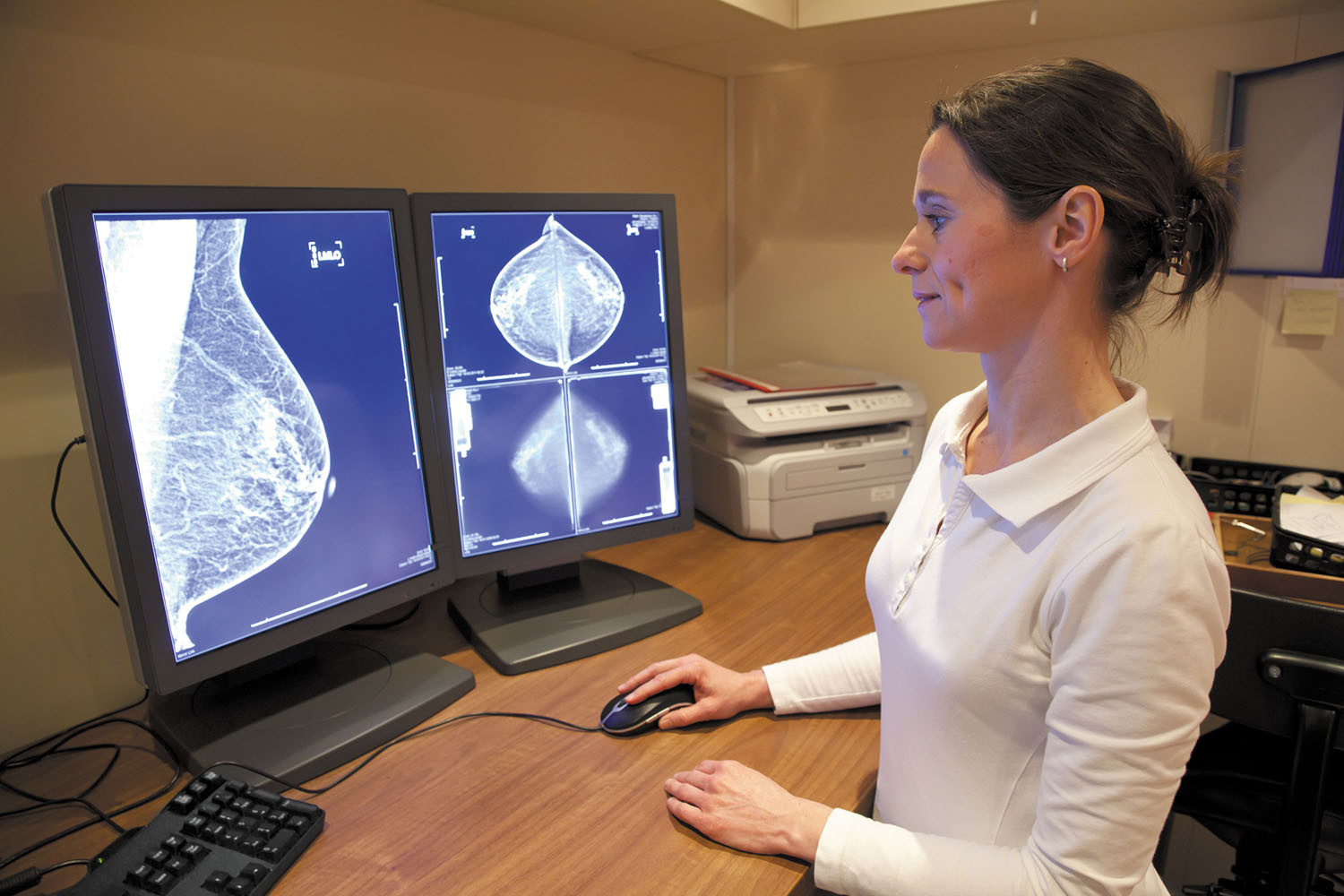
Dealing with high-density breasts
The FDA may require mammography facilities to notify patients about this breast cancer risk factor, but women don't know what to do with this information.
Do you know how dense your breasts are? If you don't, a new proposal by the FDA may mean you will soon find out.
The agency proposed a change that, if approved, will require mammography facilities to send letters informing women about their breast density — a measure of the proportion of active tissue versus fat in their breasts (see "The FDA proposal").
An underused option for severe depression
A new study supports the use of noninvasive brain stimulation in people with severe depression who haven't responded to medication.
If medication isn't helping to ease severe depression, nonsurgical brain stimulation may be an effective alternative to consider, according to a study published online March 27 by The BMJ. Specifically, the study found that evidence seems to back the use of repetitive transcranial magnetic stimulation (rTMS) and electroconvulsive therapy (ECT) over other, newer brain stimulation therapies.
"Many psychiatrists are unaware of these techniques, or at least don't think to recommend them for their patients," says Dr. Daniel Press, associate professor of neurology at Harvard Medical School and the clinical director for the Berenson-Allen Center for Noninvasive Brain Stimulation at Beth Israel Deaconess Medical Center. "So, studies like this are helpful in raising the banner and reminding people that these are very effective options for a large percentage of people."
Colorectal cancer screening before age 50?
On call: Measuring the PSA Is fasting necessary?
Q. I have always had my blood tests taken the first thing in the morning, before I've had breakfast. We've just moved to a new home and I'll have a long commute to the hospital, so I'd like to eat before I start out. My cholesterol has always been great, so my doctor said a light breakfast won't interfere with cholesterol tests. But he didn't know if eating would change my PSA result. What do you think?
A. At last — a PSA question with a simple, un-equivocal answer: Breakfast will not affect your PSA result, nor will lunch or dinner. In June 2005, doctors proved the point by measuring PSA levels three times over the course of a single day in 80 patients with an average age of 62 years. The samples were obtained before breakfast, after breakfast, and after lunch — and there were no changes in the PSA results.
Managing atrial fibrillation: An update
New guidelines provide advice on the role of drugs, weight loss, and procedures to cope with this common heart rhythm disorder.
The classic symptom of atrial fibrillation — a fluttering or thumping sensation in the chest — can leave you breathless, dizzy, and tired. Caused by electrical misfires in the heart's upper chambers (atria), this condition affects an estimated one in 11 people ages 65 and older.
While the symptoms of atrial fibrillation (often called afib) can be unsettling, the real danger is a heightened risk of serious strokes (see "How afib can lead to a stroke"). As many as 30% of strokes from afib prove fatal, notes Dr. Christian Ruff, a cardiologist at Harvard-affiliated Brigham and Women's Hospital.
Shortness of breath: A common symptom with many possible causes
Heart and lung issues are often to blame for breathlessness. But an accurate diagnosis may require advanced testing.
Like your heartbeat, the regular inhale and exhale of your breathing is something you usually don't notice — until something doesn't feel quite right. Shortness of breath can result from a range of problems, including an allergic reaction, an anxiety attack, or anemia. But most often, the underlying cause is a heart or lung condition.
"Because these two organ systems are so intertwined, one always affects the other," says Dr. Aaron B. Waxman, who directs the Pulmonary Vascular Disease Program at Harvard-affiliated Brigham and Women's Hospital. In fact, about 60% of people with heart disease also have a lung disease. As a result, it's not always easy to distinguish cardiac and pulmonary issues, he says.

What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up