What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Medical Tests & Procedures Archive
Articles
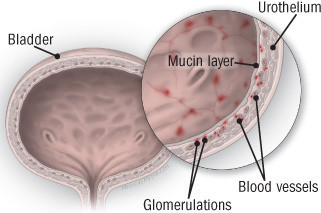
Diagnosing and treating interstitial cystitis
Also called painful bladder syndrome, this frustrating disorder disproportionately affects women.
Interstitial cystitis is a chronic bladder condition that causes recurring bouts of pain and pressure in the bladder and pelvic area, often accompanied by an urgent and frequent need to urinate — sometimes as often as 40, 50, or 60 times a day, around the clock. Discomfort associated with interstitial cystitis can be so excruciating that, according to surveys, only about half of people with the disorder work full-time. Because symptoms are so variable, experts today describe interstitial cystitis as a member of a group of disorders collectively referred to as interstitial cystitis/painful bladder syndrome. (In this article, we'll call it interstitial cystitis, or IC.)
Among the one to two million Americans with IC, women outnumber men by as much as eight to one, and most are diagnosed in their early 40s. Several other disorders are associated with IC, including allergies, migraine, irritable bowel syndrome, fibromyalgia (a condition causing muscle pain), chronic fatigue syndrome, and vulvodynia (pain or burning in the vulvar area that isn't caused by infection or skin disease).
Biotin supplements may interfere with test to diagnose heart attack
Research we're watching
Taking supplements that contain high levels of biotin (vitamin B7) can lead to falsely low results on a blood test used to detect heart attacks, according to an FDA warning issued late last year.
For adults, the recommended dietary allowance (RDA) for biotin is 0.03 milligrams (mg), which is easily obtained through a healthy, varied diet. Many multivitamins and prenatal vitamins contain far more biotin than the RDA. And some supplements — particularly those marketed to improve hair, nails, and skin — contain 20 mg, or nearly 650 times the RDA.
Is there an age limit for a colonoscopy?
On call
Q. I'm 80 and no longer do colon cancer screening. However, I recently noticed some bleeding from my rectum. Does that change my need for a colonoscopy?
A. Screening for a disease means the person has no symptoms. Since you now have rectal bleeding, a colonoscopy would be considered not a screening test, but a diagnostic test. Whether you have it now or wait to see if more bleeding occurs depends upon many factors. The most important question is whether anything found on the colonoscopy will lead to treatment that improves your quality of life.
2020 vision: Cardiology trends to watch
Several new technologies and medications that may benefit the heart are moving into cardiology care.
As regular readers of the Heart Letter know, our features tend to focus on lifestyle advice and currently available therapies for heart disease. As the new decade begins, we're also looking to the future. Editor in Chief Dr. Deepak L. Bhatt selected five promising new developments in cardiovascular research that you may be hearing more about in the coming years.
1. Digital stethoscopes
First developed more than 200 years ago, the instrument doctors use to listen to the heart and lungs has undergone some high-tech improvements in recent years. The latest digital stethoscopes feature specialized microphones and sensors that filter, buffer, and amplify sounds from the heart. The sounds are then converted to a digital signal and sent wirelessly to a smartphone, where the patterns can be visualized and further analyzed. Some models are so sensitive they can detect turbulent blood flow in the arteries of the heart, possibly enabling doctors to detect coronary artery disease. Studies assessing that potential use are currently under way.
What to do about incidental findings
They often lead to follow-up appointments and more testing.
Modern medical imaging saves lives: it can find a blocked artery, a bulging blood vessel, or a suspicious mass. But many times, an x-ray, CT scan, MRI scan, or ultrasound exam looking for one kind of problem can reveal an anomaly that's unrelated and unexpected. Such incidental findings can lead to more testing, more medical bills, and a great deal of anxiety.
"Frequently radiologists will point out something and say it's probably benign, but recommend an MRI. Once you've been told something might be abnormal, you might feel nervous until you know what it is," says Dr. Suzanne Salamon, associate chief of gerontology at Harvard-affiliated Beth Israel Deaconess Medical Center.
Why you need an annual wellness visit
The once-a-year appointment can reveal vital health information for both you and your doctor.
It's usually covered by your health insurance, it doesn't take much time, and it's a great way to learn about your present and future health.
While men often call it the yearly physical, the annual ritual is better named a wellness visit or preventive health appointment. Whatever you call it, men should still have one every year as it remains an important part of primary care, according to Dr. Asaf Bitton, executive director of Ariadne Labs and primary care physician at Harvard-affiliated Brigham and Women's Hospital.
How to make your prostate biopsy go better-before, during, and after
Before a prostate biopsy, discuss all the Image: Wavebreakmedia Ltd/Getty Images |
Here is what men need to know to minimize discomfort of a prostate biopsy and get the best results.
Have you had an HIV test?
News briefs
About half of all people in the United States living with a diagnosis of HIV (human immunodeficiency virus) are age 50 or older. But new data from the CDC suggest most Americans have never been tested for the virus (which causes AIDS, the late-stage phase of HIV infection). According to the June 28, 2019, Morbidity and Mortality Weekly Report, less than 40% of people in the United States have had an HIV test, even though the CDC recommends routine testing at least once for everyone age 13 to 64. The CDC notes that older adults sometimes aren't tested for HIV because they don't consider themselves at risk for infection or because their health care providers don't offer them the test. Older people may also mistake late-stage HIV symptoms, such as weight loss and frequent illness, for signs of normal aging. Those symptoms occur because HIV attacks the body's immune system. But a delay in diagnosis allows the virus to cause more damage. That's unfortunate, since medications can keep the infection from progressing.
If you haven't had an HIV test, talk to your doctor about whether it's right for you, no matter your age, especially if you are sexually active or have had more than one sex partner.
A blood pressure reading from a video selfie?
Research we're watching
With some smartphones, you can unlock the phone simply by showing your face. One day, a short video of your face may do far more — maybe even measure your blood pressure.
That's the premise of a novel smartphone-based technology described in the August issue of Circulation: Cardiovascular Imaging. For the study, researchers took two-minute videos of 1,328 Chinese and Canadian adults, using an iPhone equipped with transdermal optical imaging. The software measures blood pressure by detecting blood flow changes in a person's face. When compared with readings taken using a traditional blood pressure cuff, the video blood pressure readings were about 95% accurate.
Wait-and-see approaches to prostate cancer
Active surveillance and watchful waiting are the most conservative — and increasingly popular — approaches to prostate cancer management. Is one of these right for you?
Over the years, the outcome for prostate cancer has turned out to be better than expected for many men.
While prostate cancer is quite common, the risk of dying from the disease is low, even without treatment. In fact, most diagnosed men will die from something else, like heart disease. Even so, prostate cancer remains the second leading cause of cancer deaths (after lung cancer) in men, according to the American Cancer Society.

What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up