What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
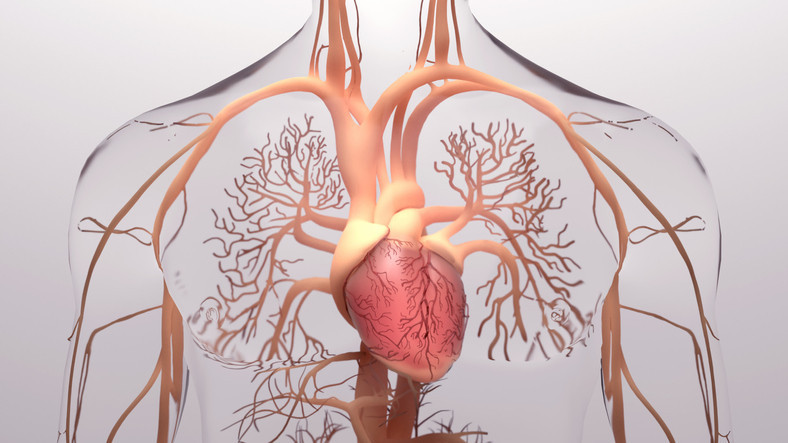
Heart Attack Archive
Articles
How good is your cardiometabolic health — and what is that, anyway?
An analysis shows less than 7% of adults in the US meet the criteria for optimal cardiometabolic health. Taking small steps to help control and improve key risk factors can reduce the odds of a heart attack or stroke.
What's driving heart attacks in younger adults?
Seven factors appear to account for most first heart attacks in people ages 55 and younger: diabetes, depression, high blood pressure, current smoking, family history of early heart attack, low household income, and high cholesterol.
What is the ideal blood pressure number?
Recent guidelines suggest a blood pressure reading of less than 120/80 mm Hg as normal. But the ideal number for individuals depends on their individual goals and whether they also have a chronic condition, such as heart disease or kidney disease.
More benefits of a Mediterranean diet
A randomized trial published May 14, 2022, in The Lancet found that people with heart disease who ate a Mediterranean diet for seven years had a 26% lower risk of having a heart attack or stroke, compared with people who ate a low-fat diet.
Happy heart syndrome: Even positive stress can affect the heart
Grief, fear, conflict, or other negative emotions can lead to an unusual type of heart attack, commonly known as broken heart syndrome. Rarely, positive emotions can also trigger the problem—and this "happy heart syndrome" may be more prevalent among men.
Too little sleep may be hard on your heart
Not getting sufficient sleep may harm the cardiovascular system by triggering physiological and hormonal changes that increase blood pressure, blood sugar, and blood levels of substances that indicate inflammation. People who don't regularly get at least seven hours of sleep a night should assess their daily habits to look for ways to improve, such as by establishing an earlier bedtime and turning off all electronic devices at least an hour before bedtime.
Preventing repeat heart attacks: Mediterranean vs. low-fat diet
For people with heart disease, a Mediterranean diet prevents future heart problems better than a low-fat diet.
Stroke risk rises in people who develop depression after a heart attack
A 2022 study found that people who have depression after a heart attack are nearly 50% more likely to suffer a stroke compared with heart attack survivors who don't develop depression.
Heart problems and the heat: What to know and do
High temperatures raise risk for heat exhaustion and heat stroke, and also stress the cardiovascular system, making the heart work harder. If you have a heart condition, here's how to keep cool and protect yourself when temperatures rise.
What is acute coronary syndrome?
Acute coronary syndrome (ACS) refers to a spectrum of conditions defined by a sudden reduction in blood flow to the heart. Most often, the underlying cause is a gradual buildup of fatty deposits called plaque inside the arteries supplying the heart. ACS includes two distinct types of heart attacks, known as STEMI and NSTEMI, and a serious condition called unstable angina that's often a prelude to a heart attack. All warrant immediate medical attention.

What are somatic workouts?

How to curb your stress eating

How to spot Parkinson’s disease symptoms

8 simple ways to reduce ultra-processed foods in your diet

Heart failure symptoms in women: How they’re different

GERD diet: Foods to avoid to reduce acid reflux

Strong is the new skinny

Everyday habits that sneakily weaken your bones

Don’t wait to get help for back pain

Correcting how you walk may ease osteoarthritis knee pain
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up