Above-normal blood sugar linked to dementia
There are many reasons to keep your blood sugar under control: protecting your arteries and nerves are two of them. Here’s another biggie: preventing dementia, the loss of memory and thinking skills that afflicts millions of older Americans.
A study published today in the New England Journal of Medicine shows that even in people without diabetes, above normal blood sugar is associated with an increased risk of developing dementia. This finding goes beyond previously seen links between diabetes and dementia. “It establishes for the first time, convincingly, that there is a link between dementia and elevated blood sugars in the non-diabetic range,” says study author Dr. David Nathan, a Harvard Medical School professor and the director of the Diabetes Center and Clinical Research Center at Massachusetts General Hospital.
Dr. Nathan teamed up with researchers across the country to look at blood sugar levels in more than 2,000 older adults—the average age was 76—taking part in the Adult Changes in Thought study. The vast majority of the study participants did not have diabetes. What the researchers found is that any incremental increase in blood sugar was associated with an increased risk of dementia—the higher the blood sugar, the higher the risk.
Why? There are only theories. “The speculation is that elevated blood sugar levels are causing more vascular disease, but it may be other metabolic issues. For example, people with elevated blood sugar often have insulin resistance which may be the link that affects our brain cells,” says Dr. Nathan.
The study does not prove that high blood sugar causes dementia, only that there is an association between the two. For that reason, don’t start trying to lower your blood sugar simply to preserve your thinking skills, cautions Dr. Nathan. There’s no evidence that strategy will work, although he says it should be studied.
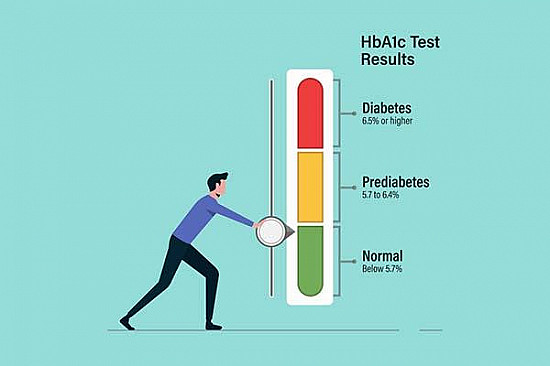
But it is worth keeping an eye on your blood sugar to try to avoid developing type 2 diabetes. This disease is at epidemic proportions. Almost 26 million Americans—one in 12—have diabetes. High blood sugar is hallmark of this disease. Normal blood sugar is under 100 milligrams per deciliter of blood mg/dL after an eight-hour fast. You have diabetes if your blood sugar is 126 mg/dL or higher after a fast. People with a blood sugar reading of above 100 but below 126 have what’s called prediabetes. Nearly 80 million Americans are in that camp.
Excess blood sugar is a problem because it can lead to a variety of health problems including heart, eye, kidney, and nerve disease.
Taming blood sugar
What if your blood sugar is above normal? There’s good news in that department: You can lower your blood sugar by exercising and, if needed, losing weight. Shifting to a healthier diet with more vegetables, fruits, and whole grains and cutting back on highly refined grains can also help.
Try to get 150 minutes per week of moderate intensity activity, such as brisk walking. If that’s daunting, know that even a little activity can make a big difference in lowering blood sugar levels. Short but frequent walking breaks—as brief as a minute and forty seconds every half hour—can lower blood sugar. So can taking a walk after a meal.
And it doesn’t always have to be official “exercise.” Try taking the stairs more often, parking farther away from the store, and getting up and moving if you’ve been sitting too long. “It’s common sense,” says Dr. Nathan. “The more active you are and the less sedentary, the more likely it is that your muscles can uptake glucose, and the insulin you make will be more effective.”
Also helpful is cutting back your intake of highly refined carbohydrates, especially foods with added sugars such as sucrose, high fructose corn syrup, and also molasses, cane sugar, corn sweetener, raw sugar, syrup, honey or fruit juice concentrates. The American Heart Association recommends no more than 100 calories from sugar or six teaspoons of sugar per day for women, and 150 calories or nine teaspoons of sugar per day for men. If you’re in the prediabetic or diabetic range, you’ll want to work with a dietitian to determine your exact needs.
Making these changes is an investment, to be sure. But the payoff—better physical and mental health—is definitely worth it.
About the Author

Heidi Godman, Managing Director
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.