Brief brain attacks: Short symptoms, long consequences
A transient ischemic attack (TIA) may foretell a gradual decline in thinking and memory.
- Reviewed by Christopher P. Cannon, MD, Editor in Chief, Harvard Heart Letter; Editorial Advisory Board Member, Harvard Health Publishing
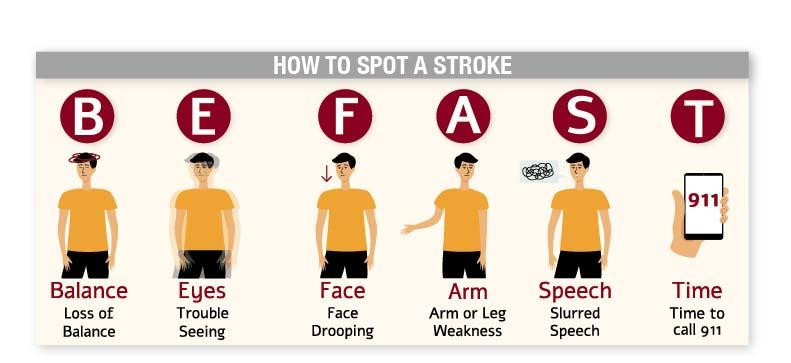
Imagine that you suddenly can’t see normally, or your speech becomes garbled, or one of your legs goes weak or numb. These unsettling symptoms are among the classic warning signs of a stroke and should prompt an immediate 911 call (see illustration).
Yet these symptoms may be short-lived, lasting just minutes. When that happens, it’s either a transient ischemic attack, or TIA (which leaves no visible evidence of damage on an MRI scan) or a ministroke (which may cause subtle changes in brain tissue visible on MRI). Now, a new study finds that a first-time TIA can lead to the same long-term decline in thinking and memory problems as a stroke.
The study included more than 30,000 people ages 45 and older who had never had a stroke or TIA and were then followed over an average of 14 years. Researchers compared the cognitive changes among three groups of people: those who experienced a stroke during the study period, those who had a TIA, and those who had neither.
After adjusting for factors like age and other health conditions, they found that after a stroke, people immediately experienced cognitive problems, which worsened over time. Those who experienced a TIA had a slower but notable drop in cognitive function compared to those without a TIA or stroke. The findings, published in the April 2025 issue of JAMA Neurology, suggest that TIAs are more foreboding than once assumed.
Trustworthy findings
Earlier research had hinted at this phenomenon, but the new study’s careful design lends credence to the results, says Dr. Andrew Budson, chief of Cognitive and Behavioral Neurology at the VA Boston Healthcare System and a lecturer in neurology at Harvard Medical School. All the participants who had TIA or stroke symptoms had a specialized MRI scan capable of detecting very tiny ministrokes, he explains. “People classified as having a TIA had no lesions on their MRI. That proves that the TIA was truly transient and not a small stroke that resolved but still caused damage to the brain,” he says. This strict definition of a TIA fits with the way a neurologist views the brain, he adds.
Another advantage: researchers were able to capture the trajectory of each person’s thinking and memory abilities before and after the TIA, which showed a change in the slope of the decline starting right after the TIA. “That means we cannot assume that these people had an underlying, alternative cause of their cognitive problems that was simply unmasked by the TIA,” Dr. Budson says.
How TIAs change the brain
Exactly how a TIA leads to cognitive changes isn’t clear. One theory is that the temporary interruption in blood flow that happens during a TIA alters the blood-brain barrier. The resulting inflammatory response may affect amyloid proteins in the brain, triggering a cascade of changes resulting in Alzheimer’s disease. Another possibility is that when a person has a TIA, they’re likely to have future TIAs and strokes. This can lead to vascular dementia, which results from longstanding, cumulative damage to blood vessels that supply the brain regions important for various thinking abilities.
Take-home messages
If you or a loved one has a TIA, make an appointment with a neuropsychologist to have baseline cognitive testing, Dr. Budson suggests. “That way, you can start addressing any abnormalities right away with a neurologist and be ready for follow-up testing if things go downhill over time,” he says. Be sure to control all your risk factors for heart attack and stroke by keeping your blood pressure, blood sugar, and cholesterol levels in check. If the neurologist suspects Alzheimer’s disease, the new amyloid-targeting therapies approved for early-stage Alzheimer’s could be an option, as the study authors suggest.
What else can you do to protect your cognitive abilities? “There’s no doubt in my mind that engaging in aerobic exercise should be your No. 1 priority,” Dr. Budson says. A less obvious recommendation is to have your hearing tested and get hearing aids if you need them. Hearing loss is a risk factor for dementia, probably because trouble hearing can lead to social isolation, Dr. Budson notes. People stop going to social events and can become withdrawn and lonely, leaving them more prone to cardiovascular disease as well as dementia.
Image: © sabelskaya/Getty Images
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
About the Reviewer

Christopher P. Cannon, MD, Editor in Chief, Harvard Heart Letter; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.