A new approach to peripheral artery disease
GLP-1 medications are being studied as a way to ease symptoms of this common and debilitating condition.
- Reviewed by Anthony L. Komaroff, MD, Editor in Chief, Harvard Health Letter; Editorial Advisory Board Member, Harvard Health Publishing
Walking can be excruciating for people with peripheral artery disease (PAD) in the legs. The condition reduces the amount of blood that reaches leg muscles, making even a short trip to the mailbox painful and challenging.
Doctors have had few ways to relieve symptoms. But new evidence suggests that GLP-1 receptor agonists, the blockbuster drugs that treat diabetes and obesity, might help. “This is something we’re watching very closely. It’s unclear if the medications are actually treating PAD or if they’re controlling underlying conditions,” says Dr. Nikolaos Zacharias, a vascular surgeon at Harvard-affiliated Massachusetts General Hospital.
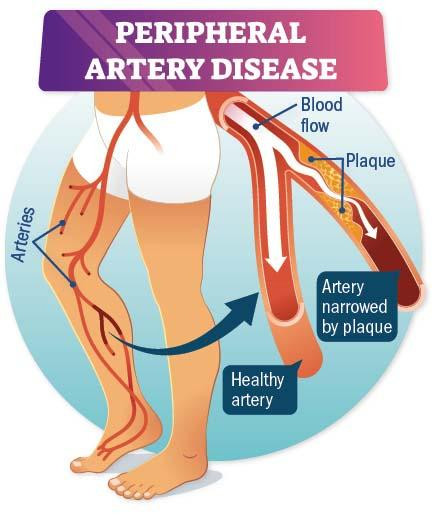
Peripheral artery disease
Peripheral artery disease is a common circulatory problem in which narrowed arteries reduce blood flow to your limbs. Image: © VectorMine/Getty Images |
PAD is risky
Just like arteries of the heart, the walls of arteries elsewhere in the body — typically in the legs, but also in the arms or abdomen — can become stuffed with fatty deposits and plaque, a condition called atherosclerosis. The narrowed arteries leave little room for blood flow, short-changing the muscles of oxygen and nutrients they need. This leads to claudication, a painful impairment that occurs with activity and gets better with rest.
If you have PAD, there’s also a good chance you have atherosclerosis in your heart and brain arteries, increasing your risk for heart attack or stroke. PAD raises risks for skin ulcers, gangrene, and limb amputation, too.
Diagnosis and treatment
Doctors diagnose PAD with a physical exam, a test (called an ankle-brachial index) that compares blood pressure in your arms and legs, and sometimes an ultrasound exam to see if a specific artery is blocked.
The main way to treat PAD is with a walking program supervised by a physical therapist. The exercise helps reroute blood flow around blocked arteries. “That, in combination with smoking cessation and controlling diabetes, cholesterol, and high blood pressure, often leads to results within six months. If not, we might need to do a procedure that improves blood flow,” Dr. Zacharias says.
What about medication?
Only a few drugs are approved to increase blood flow to the legs, and just one — cilostazol — is a top choice recommended by guidelines. Unfortunately, the medication doesn’t work for everyone. “One out of two people who take cilostazol feels improvement. But it doesn’t treat the cause, it has a lot of side effects, and it’s not safe for people with heart failure,” Dr. Zacharias says.
So the idea that GLP-1s might ease PAD symptoms is encouraging. Most recently, a randomized controlled trial published May 3, 2025, in The Lancet found that a GLP-1 boosted walking ability and quality of life in people with PAD and diabetes.
The study involved about 800 people (average age 68) with diabetes, PAD, and mild pain. About half of them were directed to take 1 milligram per week of the GLP-1 drug semaglutide, and the other half took a fake medication (placebo). After one year, people in the GLP-1 group could walk 13% farther, had more pain-free walking, had lower blood sugar, and lost more weight than people in the placebo group.
“It could be that at the same time the medication is decreasing inflammation in the body, it might also be reducing plaque in the blood vessel wall,” Dr. Zacharias says. “We just don’t know yet.”
What you should do
If you have PAD, you might be wondering if it’s time to ask your doctor about taking a GLP-1 drug. Dr. Zacharias says it might be appropriate in certain instances. “The indications for prescribing GLP-1s are for diabetes, obesity, some cases of heart disease, or some cases of sleep apnea—not an isolated case of PAD. However, if a patient with PAD also has diabetes or obesity, then yes, I might prescribe a GLP-1. I already have in selective cases,” he notes.
That careful approach will likely remain standard until there’s much more evidence that GLP-1s help people with PAD. “GLP-1s have side effects, especially gastrointestinal problems,” Dr. Zacharias says. “We want to improve your lifestyle so that, for example, you can make it to the mailbox without leg pain. But we may not know for years if GLP-1s are a safe and effective treatment for PAD.”
About the Author

Heidi Godman, Managing Director
About the Reviewer

Anthony L. Komaroff, MD, Editor in Chief, Harvard Health Letter; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.