Cholesterol: Understanding HDL vs. LDL
There are two main types of cholesterol: high-density lipoprotein (HDL) and low-density lipoprotein (LDL). (Lipoproteins are made of fat and protein, and serve as vehicles for your cholesterol to travel through the blood.) Cardiologists are often asked about low-density lipoprotein (LDL) versus high-density lipoprotein (HDL). The difference is important to understand.
What does HDL cholesterol do?
HDL clears from the body via the liver. HDL may therefore prevent the buildup of plaque, protect your arteries, and protect you from atherosclerotic cardiovascular disease. It is considered the "good" cholesterol, and higher levels are better. A good goal to aim for is higher than 55 mg/dL for women and 45 mg/dL for men. The higher your HDL cholesterol numbers, the lower your risk is for heart disease, vascular disease, and stroke.
How to increase HDL cholesterol
Although HDL levels are driven by family genetics, you can improve HDL levels in three key ways:
- If you are a smoker, research clearly shows that quitting smoking can increase HDL.
- Adopting a heart-healthy diet low in fat and high in fiber can also modestly raise your HDL.
- Aerobic exercise can also have positive effects on HDL. Have trouble exercising? Find a buddy; research shows it helps motivate you. That exercise can be as simple as increasing the amount of walking you do (for the sake of exercise, not a stroll) each week.
Lastly, although primarily used to decrease high LDL, some statin medications may potentially increase HDL levels moderately. Any medical treatment option should be discussed with your doctor. Importantly, high HDL does not protect you from the untoward effects of high LDL.
What does LDL cholesterol do?
LDL is considered the "bad" cholesterol. It carries cholesterol to your arteries, where it may collect in the vessel walls and contribute to plaque formation, known as atherosclerosis. This can lead to decreased blood flow to the heart muscle (coronary artery disease), leg muscles (peripheral artery disease), or abrupt closure of an artery in the heart or brain, leading to a heart attack or stroke. Over a third of the US population has high LDL cholesterol. Diagnosis is made via blood testing, so if you don't check, you won't know.
For LDL, the lower the number the better. A good goal to keep in mind is less than 130 mg/dL if you don't have atherosclerotic disease or diabetes. It should be no more than 100 mg/dL, or even 70mg/dL, if you have any of those conditions or high total cholesterol. It's very important to set your own target cholesterol levels with your doctor. Obesity, a large waist circumference, a sedentary lifestyle, or a diet rich in red meat, full-fat dairy, saturated fat, trans fats, and processed foods can lead to high LDL cholesterol.
How to lower LDL cholesterol
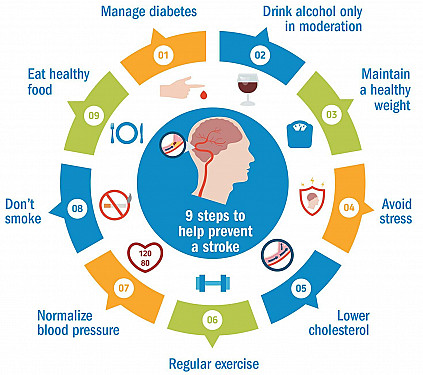
Lifestyle and diet changes are the main ways to prevent or lower high LDL. A trial of eating a low-fat diet, regular aerobic activity, maintaining a healthy weight, and smaller waist circumference is an appropriate first step. It is best to set a timeline to achieve your goals with your doctor. In some cases, if those lifestyle changes are not enough, your physician may suggest a cholesterol lowering medication, such as a statin. If you are considering over-the-counter herbal or ayurvedic medications for cholesterol, please discuss those with your physician first as well.
Rarely, very high LDL is genetic and passed down in families. This is called familial hypercholesterolemia and is caused by a genetic mutation that decreases the liver's ability to clear excess cholesterol. This condition can lead to very high LDL levels, and heart attack or stroke at a young age in multiple generations. Those individuals may require special medical treatment for prevention and treatment of atherosclerotic cardiovascular disease.
Remember, knowledge is the first step. If you don't know your cholesterol levels, get tested. That will give you and your physician a starting point for lifestyle changes and medications if needed. In the meantime, adopt a heart-healthy lifestyle, and do it with friends and family no matter their ages. There's no time like the present to prevent heart disease.
About the Author

Ami Bhatt, MD, FACC, Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.