Diabetes drug pioglitazone could get personal: Neither panacea, nor peril

When I was in training, one of my beloved mentors declared, “I never use a drug until it’s been on the market for 20 years.” I was young enough then that I couldn’t fathom being a doctor for 20 years, let alone waiting two decades to use a new drug. As my career has progressed, I’ve seen many new drugs released to the market. Some of them are truly miraculous, bringing people longer, healthier, and more productive lives. Many of them have not withstood the test of time. More than a few have even been taken off the market. Even though the Food and Drug Administration diligently reviews each new medicine before it’s approved for use, we often learn much more about a drug after its release into the general population.
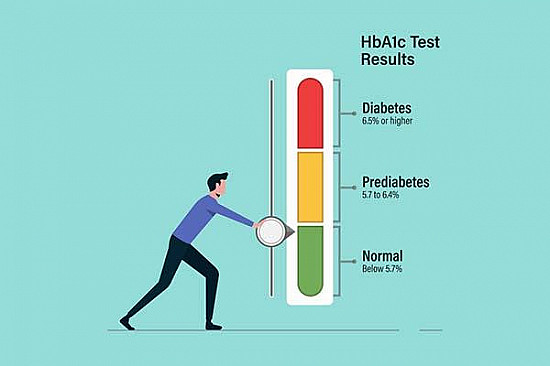
I reflected on that memory when I read a recent editorial in The New England Journal of Medicine (NEJM) about insulin resistance. In his editorial, the author tells us of the “long, strange trip” of a class of medications called thiazolidinediones, which help people who have type 2 diabetes or pre-diabetes to be more sensitive to the insulin that they make in their bodies. (Many diabetes medications work by helping the body lower its resistance to insulin in different ways.)
When they were first released, these medicines were widely accepted and adopted. We do, after all, have an epidemic of obesity and diabetes in the United States, and they seemed to work very well for people. They seemed a great alternative to insulin, which has to be injected. Then, after about 6 years on the market, these drugs began to be linked to liver disease and congestive heart failure — and maybe even cancer. Even though longer-term studies did not show that there was a definite risk of heart attack or cancer, these drugs became unpopular and fell into disuse. We were not willing to take a chance with our patients when we had other good options.
And yet, some researchers continued to wonder if there was any safe role for these very potent medications with their many positive effects, despite the concerns. The same NEJM issue as the editorial referenced above also contains a study that showed that certain carefully selected patients might, in fact, have fewer strokes if they took a medication called pioglitazone, which is in the thiazolidinedione class of medicines. Interestingly, the patients in this trial were already on extremely comprehensive stroke prevention regimens — and still they decreased their risk of a future stroke by 24%. These patients, all of whom were at risk of developing diabetes, had a slower rate of progression to diabetes as well.
What grabbed me about this story? First, it would seem that the drugs in question are neither panacea nor pariah. Pioglitazone, in fact, might a very good drug to prevent stroke in a very select population.
But, can we define that select population? That might be the most interesting tale of the past decades. Twenty years ago, we could only guess, based on certain characteristics of a patient, whether a medication would be effective. Today, we know certain people’s genetics make them better candidates for certain medications than other people. We are close to being able to tailor a medication to the patient at the level of his or her genes. When we are able to do this in an effective, safe, and efficient way, we will be able to deliver truly personalized medicine. As a clinician, I find this truly exciting. It would be wonderful to say to a patient, “This drug might have the following side effects — but I know they won’t affect you!”
My mentor may well have been right that it takes 20 years to know how a drug works and for whom it will work. He would not be surprised by the strange story of thiazolidinediones. He would undoubtedly be overjoyed by the idea that the past 20 years of laboratory and clinical research has brought us that much closer to truly personalized care.
About the Author

Lori Wiviott Tischler, MD, MPH, Assistant Professor of Medicine, Harvard Medical School
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.