4 behavioral changes to tame urinary incontinence

Although urinary incontinence is not a life-threatening medical condition, it can significantly affect quality of life. When urinary incontinence becomes bothersome, people often stop traveling, exercising, visiting family and friends — in short, people stop doing the activities they enjoy.
Surprisingly, approximately 70% of urinary incontinence can be significantly improved just by changing behavioral habits. This is called behavioral therapy. In a recent study published in Annals of Internal Medicine, behavioral therapy, either alone or in combination with medication therapy, was more effective than medication treatment alone for treating urinary incontinence.
This means if you are motivated enough to stick with a behavioral treatment program, there’s a strong chance you can improve your bladder control yourself.
Urinary incontinence: The basics
Urinary incontinence can be very minimal, leaking only a few drops. Or it can be severe, leaking so much that your pants are soaked.
The two most common types of urinary incontinence are stress urinary incontinence (SUI) and urgency urinary incontinence (UUI). SUI is the type of leaking that happens when you cough, sneeze, lift, or exercise. UUI is when you get the urge to urinate, and leak before you make it to the toilet.
Behavioral modifications help both types of urinary incontinence.
Restrict fluids
Many women do not realize that too much fluid, such as water, soft drinks, juices, and coffee, can increase the likelihood of urinary incontinence. Too much fluid can lead to an overactive bladder (OAB). The symptoms of OAB are having to urinate frequently, having to urinate urgently (possibly with urge incontinence), and having to get up throughout the night to urinate.
Drinking too much fluid can also increase the likelihood of stress incontinence. A bladder is like a balloon filled with water, with a rubber band (the urethral sphincter muscle) wrapped around the neck. If the balloon is really full and you squeeze it, the water will leak or squirt out.
It is best to keep your fluid intake in the range of 48 to 64 ounces per day. That’s just six to eight 8-ounce glasses. Spread your fluid intake throughout the day.
Limit caffeine
Caffeine is another important contributor to urinary incontinence. Caffeine stimulates the kidneys to make more urine at a faster-than-normal rate. Bladders do not like to be filled rapidly. They react by becoming overactive, or squeezing down (spasming) when they shouldn’t, making it more likely that you’ll experience UUI.
Try to minimize or even stop your caffeine intake. If you have to have some caffeine, limit your intake to 8 ounces per day.
Train your bladder
If you need to urinate frequently, you can treat this with bladder training. Bladder training involves spacing out your voids. So if you currently urinate every hour, make yourself wait 1 1/2 hours before your next trip to the bathroom. Once you can do that easily, make yourself wait two hours, and so on. Your goal should be three to four hours between urinating. This may take several months to achieve.
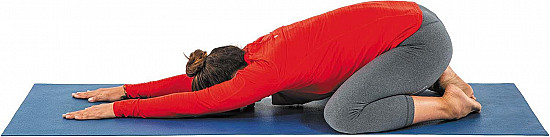
Try pelvic floor exercises
When you perform pelvic floor exercises, also called Kegels, you tighten up, or contract, the pelvic floor muscles as if you need to prevent gas from escaping. You should feel the contraction more in the back (near the anus) than in the front.
Kegels can help with both SUI and UUI, but you’ll time the exercise differently depending on which type you are trying to control.
To prevent UUI: If you feel the urge to void and do not think you will make it to the toilet in time, stop, do a Kegel, wait until you feel the urgency subside, then walk to the toilet under control. The more times you do this, the more your bladder control will improve. It may take three months to see a significant improvement.
To prevent SUI: When you Kegel, the muscles pull up tissue under the urethra and help to keep the urethra closed when pressure hits the bladder. The trick is you need to Kegel before the pressure hits the bladder. This means if you are going to sneeze, you need to tighten at the moment you are inhaling. This takes practice, and it may take two to four months before you see a difference.
It is helpful to do approximately 30 Kegels every day. You can do 10 in a row (hold each Kegel for five to 10 seconds), three times every day.
If you don’t improve on your own, you can ask your PCP or gynecologist to refer you to a pelvic floor physical therapist, or search for one here. If your incontinence still does not improve, see a urogynecologist or a urologist who specializes in female bladder control problems.
About the Author

May Wakamatsu, MD, Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.