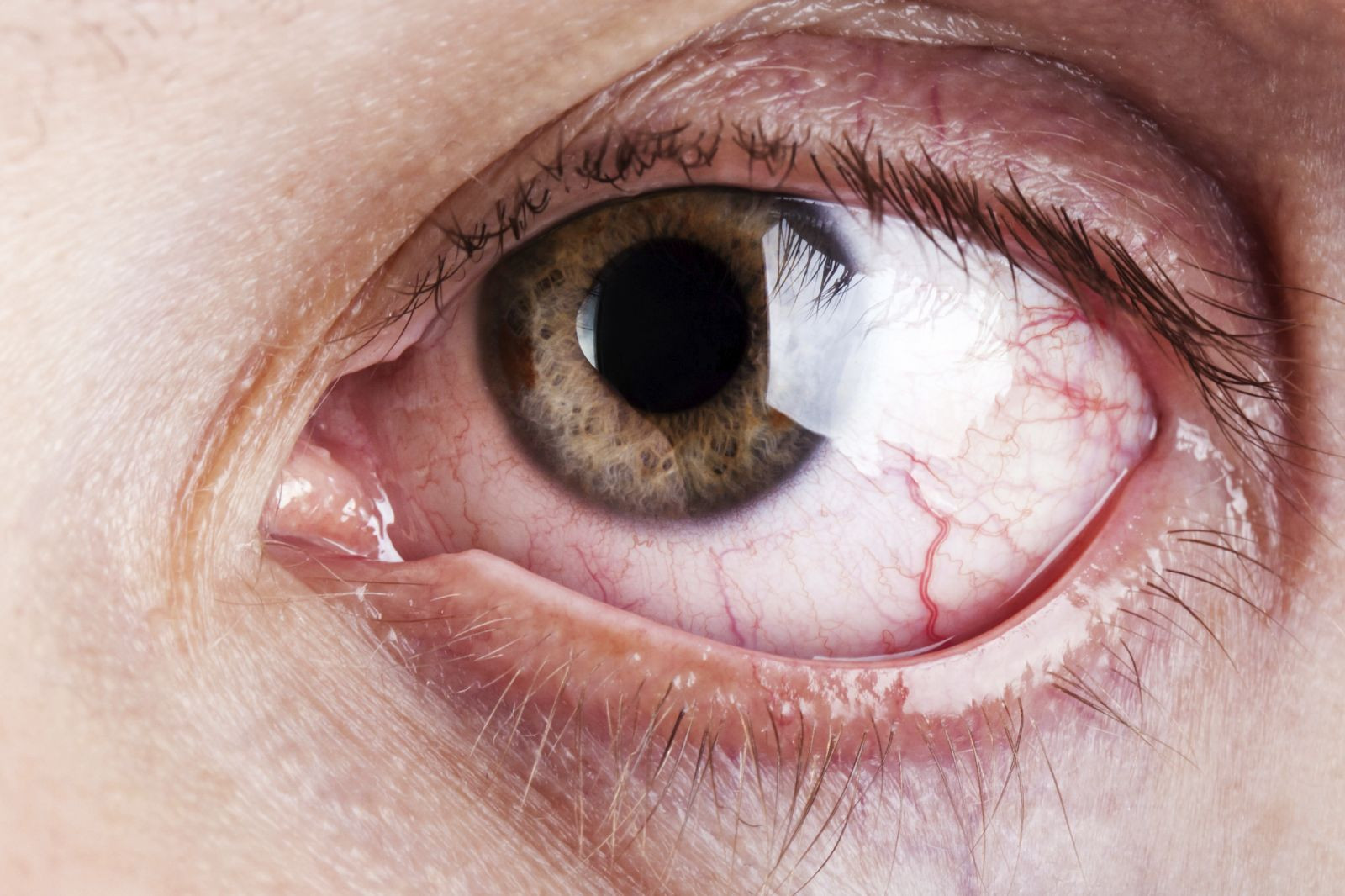
What's causing your itching, teary eyes?
Do your eyes itch after you've been near a cat? Do they puff up or run with tears when pollen is in the air?
Allergies of the eye affect about 20% to 40% of Americans each year and are on the rise. Pollens, animal dander, dust mite feces, and mold—are all triggers of allergic conjunctivitis, also called ocular allergy. Conjunctivitis is an inflammation of the conjunctiva, the lining of the eye, with symptoms such as itchy, red eyes, tearing, edema (swelling) of the conjunctiva or eyelid, and a mucous discharge.
Allergic conjunctivitis more often affects teens and young adults, but it can strike at any age. While it can be uncomfortable, uncomplicated allergic conjunctivitis is not a threat to vision.
Your doctor can diagnose allergic conjunctivitis based on your symptoms. Testing is not typically needed to diagnose the condition, but skin testing may help identify the allergens.
Treating allergic conjunctivitis
- Avoidance is your first line of defense. If you are allergic to cats, stay away from them, or at least don't touch your eyes when you're near one, and wash your hands immediately after touching one. If pollen is your allergy culprit, keep your windows closed and an air purifier or air conditioner going in pollen season.
- Artificial tears (available without prescription) can be used frequently for relief and to dilute allergens in the eye.
- Combination antihistamine/vasoconstrictor eye dropscontain both an antihistamine and a vasoconstrictor, such as naphazoline/ pheniramine (Naphcon-A, Opcon-A, Visine Allergy Eye Relief). They can be used for a few days for quick relief. You should avoid regular long-term use of these medications, as narrowing of the blood vessels of the eye and rebound redness (in which redness returns and may even be worse than before) can occur.
- Oral antihistamines can be used for occasional symptoms of allergic conjunctivitis. Newer generation of oral antihistamines include the over-the-counter medications cetirizine (Zyrtec), fexofenadine (Allegra), levocetirizine (Xyzal), and loratadine (Claritin). Keep in mind during an attack that eye drops work faster than oral medications.
For persistent symptoms, your doctor can prescribe stronger therapies. And remember to avoid rubbing your eyes. Rubbing causes mast cells in the conjunctiva to release their histamine and other inflammatory chemicals, which worsens symptoms.
To learn more about how you can minimize, manage and prevent today's most common allergies, check out Controlling Your Allergies , a Special Health Report from Harvard Medical School.
Image: ia_64/Getty Images
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.












