Why are doctors writing opioid prescriptions — even after an overdose?

A group of researchers at Boston Medical Center recently looked at nearly 3,000 patients who had survived an opioid-related overdose between 2000 and 2012. According to their recently published study, over 90% of these patients continued to receive opioid medications from doctors — even after their overdose. Given the soaring numbers of opioid-related overdose deaths and heightened scrutiny on how these medications are being over-prescribed, the study findings are alarming and disturbing.
The researchers identified almost 3,000 patients nationwide who had had a nonfatal overdose while being treated with opioid medications for chronic pain. These patients were followed for 300 days, on average, after their overdose. During those 300 days, an additional 7% of the patients overdosed a second time. In the majority of cases, the same doctor wrote the opioid prescription before and after the initial overdose.
The study did show that as a whole, patients received smaller doses of opioid medications after the overdose. But many patients were still receiving very high doses, and those receiving the higher doses were more likely to overdose yet again.
The study raises many questions. How could doctors continue to write prescriptions for opioid medications, even after an overdose? How could doctors be so ignorant to the dangers of these medications?
The problem with gaps in communication — and education
The truth is that the doctors who wrote the prescriptions probably did not know that the patients in their clinic had recently overdosed. Unless the patient was sent to an emergency room or hospital affiliated with the prescribing doctor, there is a good chance that the information about the overdose never made it back to the doctor. Indeed, doctors may never know unless the patient voluntarily discloses this information.
This communication gap is well known to those in the health care system. And this study further highlights the potential consequences of this poor communication. At the least, information about opioid overdoses must be communicated back to the prescribing doctor so that he or she can adjust pain treatment and offer addiction treatment where indicated.
The study authors give some recommendations for how to fix the communication problem. For example, the prescription monitoring program — the electronic database that doctors use to see if patients are obtaining multiple prescriptions from different doctors — could include information about overdoses. Or the insurance companies could alert the prescriber about a recent overdose.
While these measures would certainly help, the reality is that doctors have relatively little training in safely managing chronic pain and treating addiction. Whether in medical school or in residency training, very little curricular time is devoted to helping doctors safely prescribe pain medications, recognize patients at high risk for overdose, intervene when patients need to be taken off of opioids, and adequately treat opioid addiction. As such, a critical component in reducing the overprescribing of opioid medications is for medical schools and residency programs to improve how doctors are educated.
What you can do for a loved one who’s had an overdose
Family members and loved ones of those who recently survived an overdose can also help:
- If someone you love has had an overdose, make sure his or her doctor is aware.
- Consider obtaining a naloxone rescue kit, which can be used to treat an opioid overdose in an emergency situation. These kits are now available at drugstores such as Walgreens and CVS.
- If you think your loved one is addicted to opioids, encourage him or her to seek professional addiction treatment. Medication-assisted treatment with buprenorphine (Suboxone), for example, has been shown to save lives.
About the Author
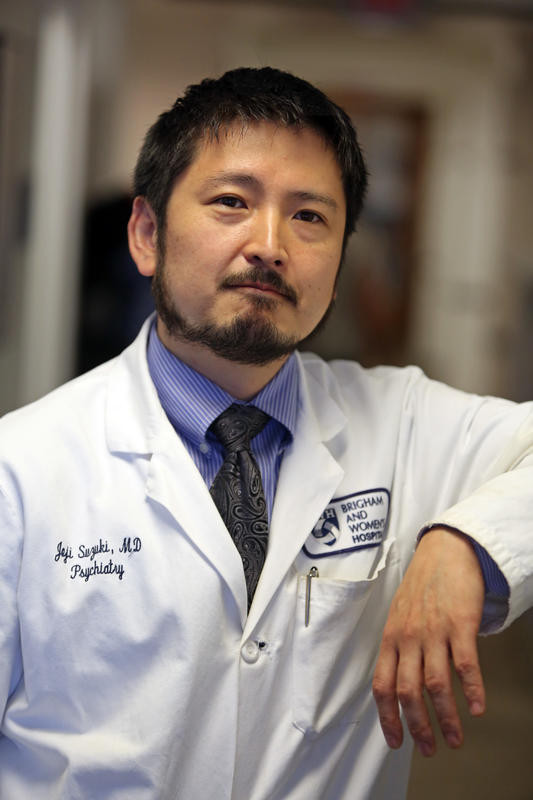
Joji Suzuki, MD
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.















