The latest on lipoprotein(a), an inherited cause of early heart disease
With promising new therapies on the horizon, cardiologists are testing more people for this biomarker, known as Lp(a).
- Reviewed by Deepak L. Bhatt, M.D., M.P.H, Former Editor in Chief, Harvard Heart Letter
About one in five people has high blood levels of fatty particles called lipoprotein(a), which doctors refer to as "L-P-little a" or Lp(a). Think of it as the evil twin of the familiar low-density lipoprotein (LDL) cholesterol, often referred to as "bad" cholesterol.
"Lp(a) particles are similar to LDL particles but with an apolipoprotein(a) molecule wrapped around each one," says cardiologist Dr. Christopher Cannon, professor of medicine at Harvard Medical School. Lp(a) accelerates the buildup of fatty plaque inside arteries and inflammation even more than LDL does. A high Lp(a) level may double or even triple a person's risk of a heart attack. It also raises the risk of stroke and is linked to a narrowing of the aortic valve (aortic stenosis).
So why have most people never even heard of Lp(a)?
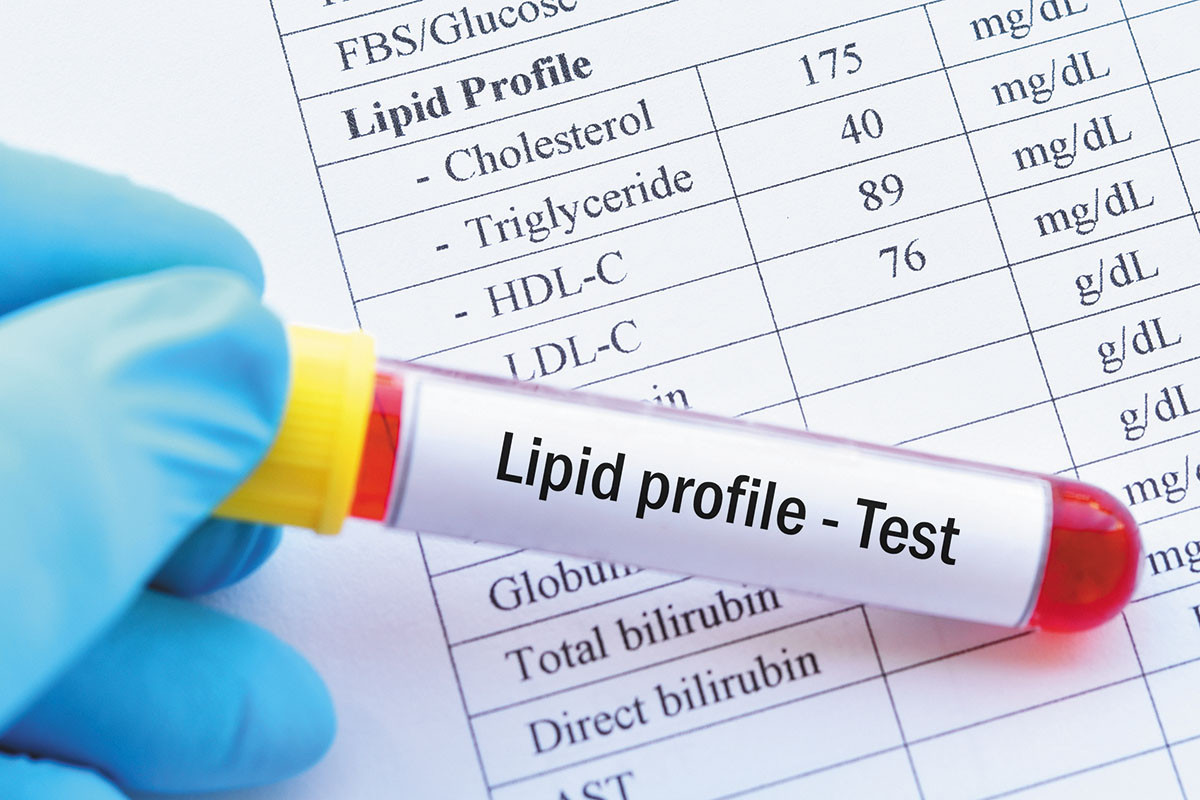
For starters, Lp(a) isn't picked up by a standard cholesterol test. You can get a separate Lp(a) blood test, but doctors haven't routinely recommended it because currently there aren't any FDA-approved drugs to lower elevated Lp(a). And because Lp(a) levels are largely genetically determined, eating and exercise habits are believed to have virtually no effect on the level in your bloodstream.
Novel RNA-based drugs lower Lp(a)The burgeoning field of RNA therapeutics uses a small piece of genetic material to interfere with and silence unwanted genes. Currently, three RNA-based drugs that shut off the gene that makes Lp(a) in liver cells are in clinical trials. The drugs, called pelacarsen, olpasiran, and SLN30, are given by injection just once every one to six months. So far, studies suggest they can lower Lp(a) levels dramatically — between 70% and 100%. The side effects appear to be limited to mild, short-lived pain at the injection site. For now, it's too soon to know whether lowering Lp(a) will prevent heart attacks and related problems, but that evidence should be available within several years. |
Testing and treatment trends
But recent clinical trials of several investigational drugs have shown promising results (see "Novel RNA-based drugs lower Lp(a)"), which have raised awareness of Lp(a). In Europe and Canada, guidelines already recommend that everyone get tested for Lp(a) at least once in their lives. In the United States, the recommendations are more conservative, with testing suggested for the following groups:
- people with premature cardiovascular disease, defined as people who've had a heart attack, stroke, peripheral artery disease, or aortic stenosis before age 55 (for men) or 65 (for women)
- people who have a father, mother, sister, or brother with premature cardiovascular disease
- people with very high LDL cholesterol (190 mg/dL or higher)
- close relatives (siblings, children, and parents) of anyone with an elevated Lp(a) level.
However, growing numbers of cardiologists support more widespread Lp(a) testing. "I'm now measuring it in most of my patients who have or are at high risk for cardiovascular disease," says Dr. Cannon. People with high Lp(a) levels often have close family members who suffered a heart attack or stroke in their 50s or even earlier. Some of these people appear to be unlikely candidates for developing heart disease because they don't have any traditional risk factors, such as high LDL cholesterol, diabetes, or high blood pressure.
A risk enhancer
But many others have one or more of those risk factors, and the high Lp(a) adds to their overall vulnerability to heart problems, says Dr. Cannon. "We think of high Lp(a) as a risk-enhancing factor that may warrant more intensive LDL lowering, in addition to paying close attention to a healthy lifestyle," he says. That means eating a mostly plant-based diet, getting regular exercise and sufficient sleep, and managing stress. Some people might benefit from aspirin and LDL-reducing drugs to lower their risk (see "The changing landscape of LDL-lowering drugs" in the April 2022 Heart Letter). People with high Lp(a) should consult a cardiologist for specific advice, says Dr. Cannon. They should also suggest Lp(a) testing for their close family members.
"I have patients who are in their 30s and 40s who find out they have high Lp(a) and are worried," says Dr. Cannon. He reassures them that he's optimistic there will be an effective therapy soon.
Image: © jarun011/Getty Images
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
About the Reviewer

Deepak L. Bhatt, M.D., M.P.H, Former Editor in Chief, Harvard Heart Letter
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.