Will new guidelines for heart failure affect you?
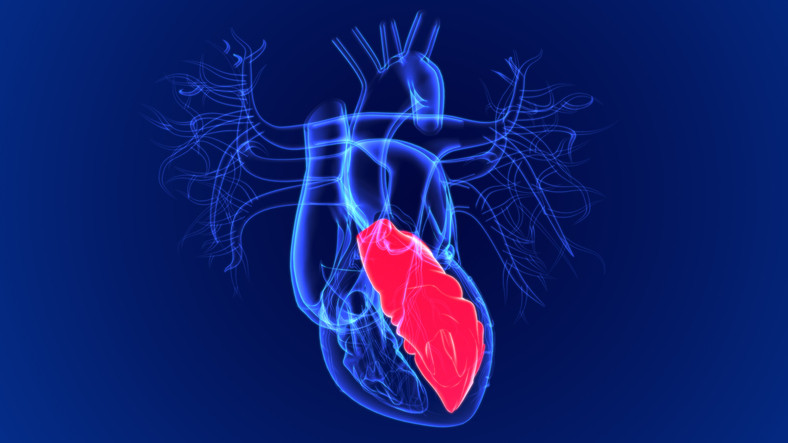
Your heart is a muscular organ with four chambers. The right atrium and right ventricle collect oxygen-poor blood from the body and pump it to the lungs. The left atrium and left ventricle collect oxygenated blood from the lungs and pump it out to the body through an artery called the aorta. In a normally functioning heart, the left ventricle sends over half the blood within it out to the body every time the heart beats. The percentage of blood the left ventricle can pump is known as the ejection fraction.
When the heart's ejection fraction is reduced, people can develop symptoms of heart failure. Heart failure due to a reduced ejection fraction (HFrEF) can impinge on a person's ability to carry out daily tasks, and affect their quality of life. It also can shorten lives. Now, recently updated expert consensus guidelines recommend new decision pathways designed to help clinicians treating people with HFrEF navigate increasingly complex therapies. If you have this type of heart failure, these changes may help you and your doctor steer a course through many important decision points. Keep in mind, of course, that treatments — and your own goals for treatment — are likely to evolve as time passes.
What are the symptoms of heart failure?
Generally, symptoms of heart failure include shortness of breath, difficulty breathing when lying flat, and swelling in the ankles. Very mild symptoms may not affect or limit activities, while people who have more advanced illness may experience symptoms with even minor activities, such as getting dressed.
How is heart failure treated?
Fortunately, a steadily increasing number of medicines, devices, and procedures help reduce heart failure symptoms and hospitalizations, and may prolong life. While these treatments offer enormous potential benefit, they can seem confusingly complex to people living with heart failure — and even to their doctors.
Good care for heart failure emphasizes choosing the right medications and taking the right doses of those medications. Identifying the best approach to help you achieve the goals you set can be a slow and complicated process, as your medical team weighs which medications to begin sooner versus later, and how and when to increase dosages, based on current evidence.
If you have HFrEF, how can the updated guidelines help you?
The recent update is aimed at guiding physicians through complex decisions on how to successfully start medicines, and choosing the right dosages for people with heart failure. This process varies depending on many factors. One piece is selecting goals, which may change over time. Goals can be big or little, short-term or long-term. For some people, it may be their ability to do a favorite activity, such as gardening. For others, minimizing the disruption that medications can cause in their lives is most important. For example, a person might want to avoid having to use the bathroom every hour in the middle of the day.
Further, the update notes that two groups of people — older adults and those who identify as African American — have been underrepresented in studies examining many treatments for heart failure. So, we don't currently know if the optimal dose of a given medicine might differ for these groups. In some cases, very limited data is available to show whether a drug works for certain populations. While acknowledging limitations, the update shares specific guidance for people in these groups. It also identifies ways to monitor whether the treatments chosen are working well.
When should you see an expert in heart failure?
While you may receive much of your care for heart failure within a primary care practice, in some instances it's wise to see an expert to decide on the best path to take. Ask your doctor whether a referral to a cardiologist experienced in heart failure could be helpful at specific points. For example, it can help to see a cardiologist
- when you are first diagnosed, to ensure that appropriate diagnostic testing has been done, and to choose a treatment plan that will be best for you.
- if you experience persistent symptoms that limit your ability to function, have repeated hospitalizations for heart failure, or develop related health issues, such as worsening kidney disease or heart rhythm disorders.
Do you find it hard to follow your treatment plan for HFrEF?
Often, even the best medical advice for managing heart failure is hard to maintain for many reasons. Medicines may have side effects, like fatigue. The cost and logistics of taking several medicines at different times may be challenging. Not surprisingly, as many as half of people following a treatment plan for HFrEF aren't able to take medicines consistently as prescribed — so if you're finding it hard, you're not alone.
Unfortunately, not taking medicine as often as needed or at the dose needed can affect your health. So, talk to your doctor to see if there are ways to address the challenges that make it hard to follow your plan.
Options might include
- getting larger quantities of each prescription to minimize trips to the pharmacy
- simplifying the regimen
- using pill boxes and reminders
- choosing generic medicines to lower cost, or getting assistance with copays.
Living well with heart failure depends not only on the available therapies, but on ongoing, open communication with your medical team about how you are feeling, what your goals are, and what challenges you're facing, so that together you can determine the right path forward for you.
About the Author

Amy Leigh Miller, MD, PhD, Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.