Urinary incontinence: Common and manageable

As a primary care doctor, I see a lot of women dealing with the inconvenience, discomfort, and embarrassment of urinary incontinence (unintended leaking of urine). Some are comfortable bringing this up right away. Others suffer needlessly because they feel too shy or awkward to mention it.
The truth is, an estimated 45% of women experience some form of urinary incontinence at some point in their lives. That's almost half of all women! It's a very big deal. Urinary incontinence can negatively affect physical and emotional well-being. For example, women may avoid going out because they're worried about having an accident away from home. Other problems include sexual dysfunction and depression.
Types of urinary incontinence
We usually think of two main categories of incontinence:
- Stress incontinence: Leaking of urine with coughing, sneezing, sex, or impact exercise, like running and jumping. This is related to damaged and/or weak pelvic floor muscles, and is common in younger women who have given birth vaginally.
- Urge incontinence: Sudden and unpredictable overwhelming urge to urinate, with leaking of small to large amounts of urine. This sometimes also goes along with needing to go often that can occur day and night. It is more common in women who are overweight, or have diabetes or other neurological issues such as dementia or strokes. The problem is thought to be due to spasms of the bladder. A lot of things can worsen symptoms, such as caffeine, diuretics ("water pills" used for high blood pressure), drinking too much fluid, and bladder infections.
The most common form of incontinence, called "mixed," has features of both these categories. But the kind of incontinence really doesn't matter. What women need to know is that there are solutions.
Get your life back by taking charge of urinary incontinence — here's how
First, talk to a healthcare provider: There are readily identifiable medical factors that can cause or worsen incontinence. Certain medications, uncontrolled diabetes, bladder infections, constipation, and menopausal changes to name a few. Your primary care doctor can help identify and treat many of these issues.
Then take care of the area: I have seen many patients who have skin rashes and infections in their genital area due to excessive moisture. Some are using menstrual pads, or even balled-up tissues or folded paper towels for their urinary leakage, or nothing at all. If moisture isn't absorbed, it will damage the skin and cause problems. Sometimes the issue is reluctance to explore the world of incontinence pads (which are now available in a variety of brands and styles), but often, sadly, it's the expense. Some insurances, including Medicaid, will cover incontinence pads; healthcare spending accounts are an option for some people as well. Barrier ointments, even plain old petroleum jelly, can help to protect skin from moisture. Daily bathing is also helpful.
Hold off on medication or surgery: Many women don't realize that lifestyle changes, physical and behavioral therapies are the preferred first-line method of treatment.
Watch the fluid intake: Limit bladder-irritating beverages such as caffeinated or acidic drinks (alcohol, coffee, black tea, green tea, sodas and seltzers with citric acid added). For women who make nighttime trips to the bathroom, decreasing fluid intake in the evening (especially alcohol) can help.
Lose a few pounds: Extra abdominal fat can create pressure on the bladder. Losing just 5% of body weight can help a lot. But even losing a few pounds can improve symptoms.
Exercise: The more physically active a woman is, the less likely she is to suffer from urinary incontinence. This may be related to better core and pelvic floor muscle tone in women with increased fitness.
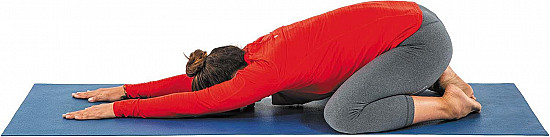
Pelvic floor exercises and physical therapy: Those Kegel squeezes can really work! They're not difficult, but it's important to do them correctly. Believe it or not, formal pelvic floor physical therapy with a trained provider can be hugely helpful. These therapists are usually women. They will take a careful history and then assess anatomy, muscle control, and strength, and then outline a guided exercise program. Once my patients get over their initial hesitation, they almost always see a benefit.
Bladder training: Scheduling bathroom visits can help women to "train" an overactive bladder. Sometimes bladder training is done along with pelvic floor physical therapy, and can be more successful that way.
And if all that doesn't help...
Talk to a healthcare provider again. There are several medications that may help. For women with postmenopausal vaginal and vulvar changes (called atrophy), an estrogen cream or ring can help a great deal. It may take as long as four months to see an effect, and though topical estrogen is low-risk, hormone therapy is not for everyone. There are also medications specifically for urinary incontinence, though frankly none are likely to be a cure. In fact, all the pills we see advertised (such as anticholinergics, the most commonly prescribed) only result in one or two less incontinence episodes per day, at best. Plus, there are many side effects, such as sleepiness, confusion, dry eyes, dry mouth, and constipation. These medications are especially dangerous in the elderly. Even the newer medications aren't much different in terms of efficacy and side effect profile.
The important takeaway messages about urinary incontinence
Here's what women really need to know:
- If you suffer from incontinence, know that you are not alone.
- Talk to your healthcare provider about it. Make sure there's nothing else going on that should be addressed.
- Try lifestyle changes, behavior and physical therapies first, and second, and third.
- Be cautious with all medications, and weigh risk, benefits, and side effects carefully with your doctor.
Resources
Evaluation of women with urinary incontinence. UpToDate, September 14, 2017.
Treatment of urinary incontinence in women. UpToDate, August 28, 2017.
Urinary Incontinence and Associated Female Sexual Dysfunction. Sexual Medicine Reviews, October 2017.
MGH Primary Care Office Insight chapter on Urinary Incontinence in Women (Mary Hohenhaus, MD and Shana Birnbaum, MD, Specialist Reviewer: May Wakamatsu, MD)
Nonsurgical Management of Urinary Incontinence in Women: A Clinical Practice Guide from the American College of Physicians. Annals of Internal Medicine, September 16, 2014.
Effectiveness of pelvic floor muscle training in treating urinary incontinence in women: A current review. Actas Urologicas Espanolas, June 2016.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.