Sepsis: When infection overwhelms

When I was a doctor in training I was involved in a very sad case, the unexpected death of a patient, a woman in her fifties who had diabetes.* She had been seen in the clinic and diagnosed with pneumonia only two days before her passing. The diagnosis was correct, as well as the prescribed antibiotics. But she had been sent home, and her condition deteriorated quickly. By the time her family brought her into the emergency room, she was in septic shock.
What is sepsis?
What does it mean to be in septic shock? Sepsis is when the body's response to a serious infection gets out of control. As the illness progresses, the cells of the immune system release a cascade of chemicals that eventually cause massive inflammation and can lead to organ malfunction, shock ("septic shock"), and death. The death rate from sepsis can range from 25%50%.
Generally, infections of the lungs (like pneumonia), urinary tract, abdomen, and skin are more likely to cause sepsis, and certain bacteria are the most common culprits.
Who is most likely to develop sepsis?
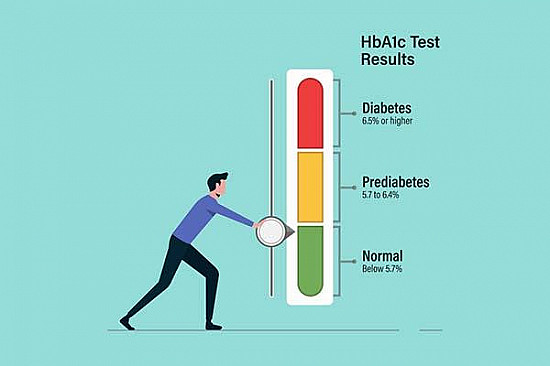
Some people are more likely to develop sepsis: those older than 65, infants younger than one year, and anyone with a weakened immune system are all particularly susceptible. The immune system can be weakened by certain medications, such as steroids, chemotherapy, or drugs to prevent transplant organ rejection; many chronic diseases such as diabetes, heart failure, and kidney failure hinder the immune system as well. This makes it easier for germs to multiply, and infections can quickly become overwhelming,
In the case of our patient above, she had a lung infection with a strain of bacteria called pneumococcus, which commonly causes pneumonia. She also had a weakened immune system due to diabetes, and she had declined the pneumonia vaccine. These factors made her very vulnerable to sepsis, and she should have been admitted to the hospital from the clinic for more aggressive treatment and closer monitoring, rather than sent home.
Since this case almost two decades ago, I have seen multiple patients who developed sepsis. Each case is very different, but they are all pretty much seared into my memory. (And, for the record, no one under my immediate care has died.) Sepsis is an emergency. People with infections or even early sepsis often first seek the help of their primary care doctors, so I am very interested in preventing it when possible, and recognizing it quickly when it does happen.
Early recognition and treatment of sepsis are critical
The Centers for Disease Control and Prevention recently published an analysis of several hundred cases of septic shock, from 2012 to 2015. The CDC partnered with the New York State Department of Health and Emerging Infections Program to examine the records of 246 adults and 79 children diagnosed with sepsis to see what factors contributed, and how it could have been prevented.
One huge factor is whether people had been properly vaccinated, and specifically whether they had gotten a pneumonia vaccine. The CDC authors state: "pneumonia is the most common infection causing sepsis, and vaccination is an important and highly effective prevention strategy." Appropriate vaccination can prevent the worst infections from starting in the first place.
Another key finding in the CDC study was that approximately 72% of these patients had had contact with the healthcare system in the days prior to their illness. Many of these patients had chronic health problems, and so would be in medical offices or hospitals more often than healthy people. But, the report suggests that contact with the medical system itself could pose a risk for infections (and therefore sepsis), for example from hospital-acquired infections of intravenous lines and urinary catheters. Another important finding was that there may have been opportunities for providers to intervene earlier in the infections. With sepsis, early recognition and treatment is essential; once septic shock sets in, the risk of dying from sepsis increases greatly. Prevention efforts such as appropriate vaccination and minimizing hospital-acquired infection are important, and early and urgent recognition of sepsis is critical.
The CDC authors recommend that family members of susceptible patients should know the common symptoms of sepsis. These can include fevers, shaking chills, flushed skin, racing heartbeat, and confusion, among other things. As the illness progresses, the blood pressure drops dangerously low, and organs can stop functioning correctly. This can take hours or days, depending on the individual. If sepsis is at all suspected, the patient should be brought to medical attention as quickly as possible. Remember, sepsis is a medical emergency and rapid treatment can make all the difference in whether or not a person recovers.
*Yes, this example is based on a real case. But: All patient and clinical details have been altered to protect privacy. In addition, I trained over a decade ago, and my training spanned eleven years, four states, and six hospitals.
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.