Microbiome: The first 1,000 days

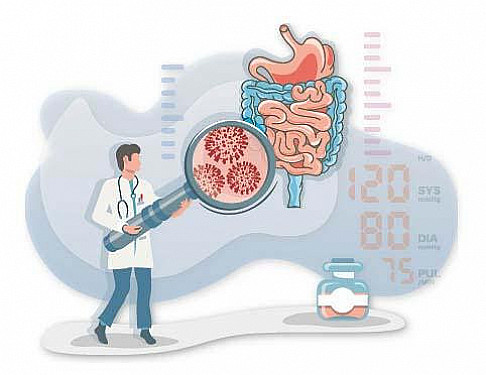
In the United States and other developed countries, we have seen a shift over the past several decades in the types of illness people struggle with. Public health campaigns around vaccination, sanitation, and judicious use of antibiotics have largely eradicated many infectious illnesses. As the nature of disease has shifted to inflammatory conditions, we've seen a striking increase in allergy and autoimmune conditions such as diabetes, obesity, inflammatory bowel disease, celiac disease, and multiple sclerosis. The microbiome — the varied and teeming colonies of gut bacteria inside of us — may be helping to drive this shift.
What is the microbiome?
Colonization occurs within the first two years of life. It passes through stages: some exposure in utero occurs with bacteria from the mother's intestine passing through the placenta into amniotic fluid. Major colonization begins with delivery, when the fetus either passes through the birth canal or is born by cesarean section. Each mode of delivery produces a different colonization pattern. Colonization is further affected by diet (breast milk vs. formula) and weaning to solid foods. Maternal illness during pregnancy and infant illness with the use of antibiotics can disrupt the process. With complete colonization at two years of life, each individual has a unique signature of billions of organisms residing principally in their colon. The nature of colonizing bacteria differs based on geographic location in the world.
Why are the first 1,000 days of life such a critical time?
Public health doctors and primary care physicians now recognize that appropriate initial bacteria colonization of the gastrointestinal tract, and good nutrition from the time of conception until the second year of life (the first 1,000 days), may profoundly affect our health during infancy and childhood through adulthood.
Recent research published in Nature Medicine underscores the importance of the large number of bacteria (billions of organisms) that colonize the intestinal tract and can contribute to the development of protective and metabolic functions in the body. In essence, the colonizing bacteria function as an additional body organ by providing protective metabolites and antibacterial substances.
During the first 1,000 days the developing fetus and newborn goes through major developmental changes in its body organs, particularly the gastrointestinal tract. The colonizing bacteria or its secretions interact with developing body functions in ways that can have long-term effects on how the infant, child, and adult respond to environmental stimuli such as diet, pets, and antibodies. Ultimately, this may help a person stay healthy or cause a chronic disease, such Type 1 diabetes or inflammatory bowel disease.
The microbiome and the process of tolerance
A newborn must appropriately colonize the intestine to accomplish reactions that are necessary to both harmful and nonharmful stimuli. Tolerance — the process of distinguishing between potentially harmful and harmless stimuli — is the means by which this occurs. An example of this is distinguishing between a harmful infectious agent such as E. coli and food substances (milk, vegetables, etc.) that aren't harmful unless an inappropriate response occurs (autoimmune disease).
However, in cases where inappropriate bacteria colonize the intestines, even harmless stimuli — such as antibiotics, food components, or harmless bacteria — could cause inflammation. This may lead to conditions such as allergy and inflammatory bowel disease.
What does this mean for expectant and new parents?
A mother at the time of conception should be healthy. Ideally during gestation, she should gain weight appropriately, continue to exercise, and hopefully be free of infections which require use of antibiotics. This results in a balanced intestinal colonization. When a baby is born by natural means, a large bolus of colonizing bacteria comes from the ingestion of the mother's intestinal and vaginal organisms. After birth, an infant rapidly colonizes its intestine under the influence of breast milk, hopefully given exclusively for the first four months of life. Breast milk contains bacteria from the mother's intestine and nutrients that stimulate proliferation of health-promoting bacteria (probiotics). Ideally an infant should be free of infections requiring antibiotics, which interfere with the natural bacterial colonization process.
In subsequent blogs I will provide further recommendations about how new parents can help their baby improve bacteria colonization during the first 1,000 days of life.
Allan Walker, MD, is the the author of Eat, Play and Be Healthy.
To learn about research in mice exploring a potential link between gut inflammation and autism, read the Gut-Brain Connection in Autism in Harvard Medicine News.
About the Author

Allan Walker, MD, Contributor
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.