Chondromalacia patella
- Reviewed by Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
What is chondromalacia?
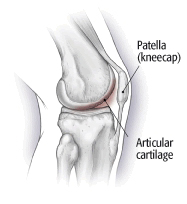
Most joints in your body are cushioned with a type of tissue called articular cartilage. This tough, rubbery tissue covers the ends of bones inside a joint. As the joint moves, the cartilage helps to cushion the bones and allows them to glide smoothly against one another.
Sometimes, the cartilage inside a joint softens and breaks down. This condition is called chondromalacia. The cartilage loses its ability to protect the ends of the bones as the joint moves. The ends of the bones can rub together, causing pain.
Chondromalacia can affect any joint, but the most common location is the underside of the kneecap (also called the patella); when affecting the knee, this condition is called chondromalcia patella. It usually begins as a small area of softened cartilage behind the kneecap that can be painful. Eventually, more of the cartilage softens, and the softened cartilage can crack or shred into a mass of fibers. In severe cases, the damaged cartilage can wear away completely, down to the undersurface of the kneecap. If this happens, the exposed kneecap's bony surface can grind painfully against other knee bones. Also, bits of cartilage can float inside the joint, further irritating the cells that line the joint. In response, these cells may produce extra fluid inside the joint (called a joint effusion).
|
|
Many different types of joint injuries and joint disorders can lead to chondromalacia. In the knee, chondromalacia is usually related to injury, overuse of the knee, and poorly aligned muscles and bones around the knee joint. These causes include:
- trauma, especially a fracture (break) or dislocation of the kneecap
- an imbalance of the muscles around the knee (some muscles are weaker than others)
- overuse (repeated bending or twisting) of the knee joint, especially during sports
- poorly aligned muscles or bones near the knee joint
- injury to a meniscus (C-shaped cartilage inside the knee joint)
- rheumatoid arthritis or osteoarthritis
- an infection in the knee joint
- repeated episodes of bleeding inside the knee joint
- repeated injections of steroid drugs into the knee.
Chondromalacia of the knee affects young adults more than any other age group. It is especially common in runners, joggers, skiers, soccer players, cyclists and other athletes who repeatedly stress their knees. Also, workers who spend a lot of time kneeling — particularly carpet layers, tile setters, and floor layers — are more likely to develop this problem.
Symptoms of chondromalacia
The most common symptom of chondromalacia is a dull, aching pain in the front of your knee, behind your kneecap. This pain can get worse when you go up or down stairs. It also can flare up after you have been sitting in one position for a long time. For example, your knee may be painful and stiff when you stand up after watching a movie or after a long trip in a car or plane.
Chondromalacia also can make your knee joint "catch" meaning you suddenly have trouble moving it past a certain point, or "give way" (buckle unexpectedly). These symptoms tend to occur when you bend your knee repeatedly, especially when you go down stairs. In some cases, the painful knee also can appear puffy or swollen.
Chondromalacia can cause a creaky sound or grinding sensation when you move your knee. However, creaking sounds during bending do not always mean that cartilage is damaged.
Diagnosing chondromalacia
Your doctor will want to know whether you have ever:
- fractured your kneecap or any other bone in the knee joint
- sprained your knee or injured your knee's meniscus (the disk-shaped, shock-absorbing cartilage inside the knee)
- had knee surgery
- had bleeding or an infection inside your knee joint
- been diagnosed with arthritis in your knee.
Your doctor also will ask about the type of work you do and your recreational and sports activities.
Your doctor will compare your painful knee with your normal one. He or she will check your painful knee for swelling, deformity, tenderness and fluid in the joint. Your doctor will look at the position of your kneecap and the alignment of your knee joint. He or she will bend and straighten your knee gently to check for creaking sounds and grinding sensations.
Your doctor may order knee X-rays. Although standard knee X-rays do not always detect chondromalacia, they can identify other causes of knee pain. If your symptoms are severe or unusual, your doctor also may order a computed tomography or magnetic resonance imaging scan of your knee.
In some cases, your doctor may want to examine your knee through a type of surgery called arthroscopy. A tube-like instrument is inserted into your knee through a small incision to allow the doctor to look at the inside of the joint and correct problems. Surgery may be the only way to be certain that the problem is chondromalacia rather than another cause that would be treated differently.
Expected duration of chondromalacia
Because articular cartilage heals poorly, chondromalacia usually is a permanent problem. However, nonsurgical treatments often can relieve knee pain within a few months. If nonsurgical treatment fails, your doctor can perform surgery to remove the area of damaged cartilage. Once this is done, most patients find that their symptoms improve.
Preventing chondromalacia
You may be able to reduce your risk of chondromalacia by preventing knee injuries and overuse of your knee joints. To do this:
- Warm up and stretch before you participate in athletic activities.
- Do exercises to strengthen the leg muscles around your knee, especially the muscles in your thigh called the quadriceps.
- Increase the intensity of your training program gradually. Never push yourself too hard, too fast.
- Wear comfortable, supportive shoes that fit your feet and your sport. Problems with foot alignment can increase your risk of knee injuries. Ask your doctor about shoe inserts that can correct alignment problems.
- If you ski or if you play football or soccer, ask your doctor or trainer about specific equipment that can help to reduce your risk of knee injuries.
- If you often kneel on hard surfaces when you work, wear protective knee pads.
Treating chondromalacia
Your doctor probably will recommend nonsurgical treatments first. These include:
- applying ice after exercise and as needed for pain or swelling
- taking a nonsteroidal anti-inflammatory drug, such as ibuprofen (Advil, Motrin and others), to relieve your knee pain and ease any swelling
- taking other pain relievers, such as acetaminophen (Tylenol), which may also relieve pain
- starting an exercise program to strengthen the muscles around your knee
- avoiding high-impact exercises
- avoiding all kneeling and squatting
- using knee tape, a brace or a special patellar-tracking sleeve to keep your kneecap aligned properly.
A physical therapist can be especially helpful to safely guide patients through these treatments.
If nonsurgical treatments fail, or if you have severe symptoms, your doctor may recommend arthroscopy to check the cartilage inside your knee. If the cartilage is softened or shredded, damaged layers can be removed during the surgery, leaving healthy cartilage in place. If necessary, your doctor also can correct the alignment of your kneecap or other parts of your knee to help to reduce wear and tear on your knee cartilage.
When to call a professional
Contact your doctor if you have knee pain that doesn't go away or if your knee catches, gives way, or looks swollen and puffy.
Prognosis
Simple nonsurgical treatments can relieve knee pain in most people with chondromalacia.
If nonsurgical treatment fails and surgery is required, studies show that most patients are satisfied with the results. Once the damaged cartilage is removed surgically, knee pain usually decreases and the knee functions better.
Additional info
National Institute of Arthritis and Musculoskeletal and Skin Diseases
National Insitutes of Health
http://www.niams.nih.gov/
American Academy of Orthopaedic Surgeons (AAOS)
http://orthoinfo.aaos.org/
American Physical Therapy Association
http://www.apta.org/
National Institute for Occupational Safety and Health
http://www.cdc.gov/niosh/
About the Reviewer

Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.