Recent Blog Articles

How do trees and green spaces enhance our health?

A muscle-building obsession in boys: What to know and do

Harvard Health Ad Watch: New drug, old song, clever tagline

Concussion in children: What to know and do

What color is your tongue? What's healthy, what's not?

Your amazing parathyroid glands

When — and how — should you be screened for colon cancer?

Co-regulation: Helping children and teens navigate big emotions

Dog bites: How to prevent or treat them

Will miscarriage care remain available?
Screening Tests for Women Archive
Articles
What to do about incidental findings
They often lead to follow-up appointments and more testing.
Modern medical imaging saves lives: it can find a blocked artery, a bulging blood vessel, or a suspicious mass. But many times, an x-ray, CT scan, MRI scan, or ultrasound exam looking for one kind of problem can reveal an anomaly that's unrelated and unexpected. Such incidental findings can lead to more testing, more medical bills, and a great deal of anxiety.
"Frequently radiologists will point out something and say it's probably benign, but recommend an MRI. Once you've been told something might be abnormal, you might feel nervous until you know what it is," says Dr. Suzanne Salamon, associate chief of gerontology at Harvard-affiliated Beth Israel Deaconess Medical Center.
Gene tests for all women with breast cancer could save money — and lives
Research we're watching
Doing genetic tests on all women with breast cancer, as compared with the typical practice of just testing those with a family history of the disease, is worth the extra cost, according to a study published online Oct. 3, 2019, by JAMA Oncology. The study authors say their findings should prompt the expansion of genetic testing to all women diagnosed with breast cancer. It's clear that testing breast cancer patients for genetic variants that raise breast cancer risk (such as BRCA1, BRCA2, and PALB2) would enable doctors to identify more women who carry these variants and who might benefit from preventive strategies. But researchers wondered whether doing so would be too costly. To answer that question, they used a computer model to analyze data from more than 11,000 women. They found that not only would the cost of testing all American women with breast cancer be balanced out by later savings on health care services, but also that just one year of testing could prevent an estimated 9,700 new cases of breast and ovarian cancer and 2,400 deaths.
Image: voinSveta/Getty Images
Should you get a home genetic test?
Direct-to-consumer tests may help predict risks to your future health. But are they worth the cost and trouble?
Image: © jxfzsy/Getty Images
Direct-to-consumer (DTC) genetic test kits are a popular way to identify a person's ancestral history, but the technology may also reveal whether someone is at risk for specific diseases and conditions, like Alzheimer's disease, heart disease, and even cancer.
"More and more people want to explore their own medical data, and a DTC genetic test is one way to begin to understand some aspects of your future health," says Dr. Robert Green, a medical geneticist at the Harvard-affiliated Brigham and Women's Hospital and director of the Genomes2People Research Program. "Yet it is important to realize that DTC testing is not the same as genetic testing in a medical context, and is not a comprehensive examination of your DNA."
Screening guidelines for women: Incontinence and cervical cancer
News briefs
Older women: Take note of two new screening guidelines. One is for cervical cancer screening. Recommendations from the U.S. Preventive Services Task Force, published online Aug. 21, 2018, by the Journal of the American Medical Association, suggest that many women ages 30 to 65 can now approach cervical cancer screening in several ways: they can get a cervical cytology (Pap) test every three years; a test for human papillomavirus (which causes most cervical cancer cases) every five years; or they can get a combination of both tests every five years. If you're older than 65, the USPSTF recommends against screening unless you haven't had adequate tests before or you're at high risk for cervical cancer. The other screening guidelines are for urinary incontinence. They come from the Women's Preventive Services Initiative and were published online Aug. 14, 2018, by Annals of Internal Medicine. The guidelines recommend that women get screened for incontinence yearly, regardless of age. "I completely agree with brief annual screening for urinary incontinence for women. A simple question can be used to screen for it, such as, 'Do you have any bothersome urinary incontinence or urinary leaking during the day or night?' If the incontinence is treated early, in some cases, it will not progress and the patient will be able to avoid more invasive, costly, risky, or time-consuming treatment options," says Dr. May Wakamatsu, vice chair of gynecology services at Harvard-affiliated Massachusetts General Hospital.
Do I need to be screened for hepatitis C?
Ask the doctors
Q. I recently saw something recommending that older Americans get screened for hepatitis C. I'm 68 years old. Should I be screened?
A. Yes. Since 2012, the CDC has recommended that all adults born from 1945 to 1965 be tested for hepatitis C, a bloodborne virus that affects anywhere from 2.7 million to 3.9 million Americans — many of whom don't know they have the condition. Hepatitis C can go undetected in the body for years, eventually leading to cirrhosis, liver damage, and liver cancer. You may be at risk even if you don't think you have any risk factors for the disease, which is most commonly transmitted today through intravenous drug use. People born from 1945 to 1965 are five times more likely than other Americans to have hepatitis C, although experts aren't sure why this is the case, according to the CDC. It's possible that some people were infected during health care procedures or blood transfusions that took place before the discovery of the hepatitis C virus. A study published in the April 2018 issue of Cancer Epidemiology, Biomarkers & Prevention found that less than 13% of these individuals have had the test. Since you're one of those who hasn't, it's a good idea to call your doctor and make a screening appointment.
Test may someday help predict diabetes risk
All women, regardless of risk, should focus on preventing diabetes.
Can a blood test act as a crystal ball, alerting you to a health hazard that may await you down the road? Researchers say they've found one that may do just that for diabetes. It could help predict whether women — even ones with no other signs of the disease — may develop the condition in the future.
In a study published online June 21 by the Journal of Clinical Lipidology, researchers showed that in many cases, a test called lipoprotein insulin resistance (LPIR) did a better job, at predicting which women would go on to develop diabetes, says Dr. Samia Mora, one of the study authors and associate professor of medicine at Harvard Medical School. In many cases, it was more accurate than traditional measures — such as
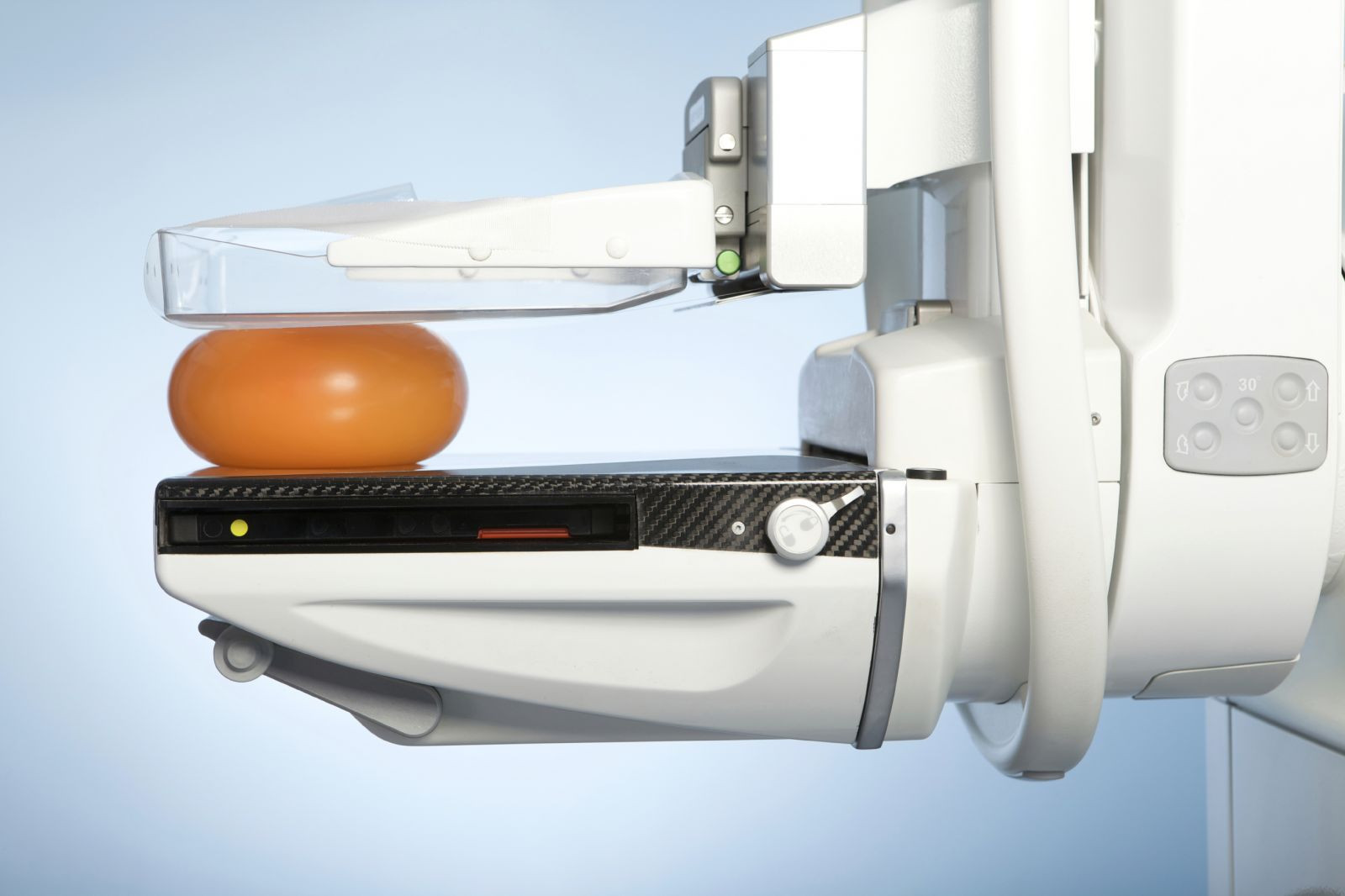
Should you still have mammograms after age 75?
The decision depends on several factors, including your breast cancer risk, life expectancy, and personal preferences.
Image: © Auremar/Thinkstock
As you get older, your body isn't the only thing that's changing. So are the guidelines for taking care of it. Breast cancer screening guidelines are a case in point. The current U.S. Preventive Services Task Force (USPSTF) guidelines recommend a mammogram every two years for women ages 50 to 75 with an average risk of developing breast cancer. For older women, the USPSTF said there isn't enough evidence of the potential risks and benefits of mammography on which to base a recommendation.
Although breast cancer is a leading cause of death in older women, women over 75 haven't been included in studies of mammography. However, there is evidence that most breast cancers detected in older women are relatively slow growing and easily treated. While a mammogram performed today might detect a cancer that would not spread or metastasize for several years, the percentage of women who survive to that point decreases with each passing year.
Heart scans: Why and when you might consider one
Coronary artery calcium tests can reveal early signs of heart disease. But they're not appropriate for everyone.
Image: © Monkey Business Images/Thinkstock
A special x-ray scan can show specks of calcium inside the walls of the heart's arteries within a matter of minutes. Known as a coronary artery calcium (CAC) scan, it offers one way to predict a person's future risk of heart disease.
However, having this test makes sense only if the results would affect a person's medical treatment. For the most part, that means it's useful primarily for people who are wavering about whether to take a cholesterol-lowering statin drug, says Dr. Ron Blankstein, a cardiovascular imaging specialist and preventive cardiologist at Harvard-affiliated Brigham and Women's Hospital.
Why isn't there a more comfortable mammogram procedure?
Ask the doctor
Q. I have been smashed, squashed, pulled, and tugged annually for 25 years. Why isn't there a better way to take a mammogram?
A. We hear you! Compression mammography has been the "gold standard" for decades for one reason — it works. Flattening the breast makes ductal tissue easier to distinguish and reduces the amount of radiation required to do so. Studies have demonstrated that it is the most effective approach to breast cancer screening.
The family history of cancer
If cancer runs in your family, there is much you can do to recognize your potential risk and catch the disease before it strikes.
Image: filipefrazao/Thinkstock
You may remember stories of your father's military service and your mother's hometown, but how much do you know about your family's medical history? In particular, do you know whether anyone on your mom or dad's side ever had cancer?
"Family history can be one of the first lines of defense in preventing cancer," says Dr. Huma Q. Rana, clinical director of the Center for Cancer Genetics and Prevention at Harvard-affiliated Dana-Farber Cancer Institute.
Recent Blog Articles

How do trees and green spaces enhance our health?

A muscle-building obsession in boys: What to know and do

Harvard Health Ad Watch: New drug, old song, clever tagline

Concussion in children: What to know and do

What color is your tongue? What's healthy, what's not?

Your amazing parathyroid glands

When — and how — should you be screened for colon cancer?

Co-regulation: Helping children and teens navigate big emotions

Dog bites: How to prevent or treat them

Will miscarriage care remain available?
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up